Breastfeeding Norms in Contemporary Society: A Case Study of Dutch Women
Mariska Hendrika Lena van der Zee, Leiden University College
Abstract
Breastfeeding protects both infants and mothers against various short-term and long-term illnesses, yet only 25 percent of Dutch mothers comply with the World Health Organisation’s recommendation to breastfeed exclusively for six months. Previous research has found various reasons for early breastfeeding cessation, such as going back to work, and societal norms seem to underlie many of these reasons. This study aims to uncover how norms and ideologies, both personal and societal, influence experiences of breastfeeding among Dutch women. A mixed-methods approach consisting of semi-structured in-depth interviews, one focus-group discussion and a survey is used. The results indicate that normativity and ideologies influence the obstacles mothers are willing to endure, and the motivation to continue or to stop breastfeeding. Moreover, contemporary societal norms influence the way in which women breastfeed in public; concealed and up to a certain age. Institutional barriers in healthcare provision appear to originate from a difference in the opinions of mothers and healthcare providers as to what good motherhood entails. Other institutional barriers include the workplace, due to employers’ and colleagues’ negative attitudes towards breastfeeding. This study shows that women are often impeded in their breastfeeding practices because breastfeeding is not normalised in every setting and due to a present gap in care provision in the Netherlands.
Keywords: Breastfeeding, Netherlands, social norms, early breastfeeding cessation, maternal and child health.
Introduction
The percentage of Dutch mothers complying with the World Health Organisation’s recommendation to breastfeed exclusively for six months is estimated to be 25 percent (OECD, 2009). Because of the short duration of breastfeeding, infants and mothers forgo important associated health benefits. A meta-analysis on the health benefits associated with breastfeeding found that breast milk protects infants against various short-term and long-term illnesses such as respiratory tract infections, gastrointestinal illnesses, and obesity later in life (Allen and Hector, 2005). Similarly, beneficial health outcomes for breastfeeding mothers include a faster recovery after childbirth, an increase in the postpartum infertility period, and a decrease in the risk of premenopausal breast cancer (Allen and Hector, 2005). Therefore, increasing breastfeeding rates would be beneficial to the overall population health.
Nevertheless, few studies provide insight into breastfeeding practices in the Netherlands, although in more recent years some attention has been paid to reasons for early breastfeeding cessation. It appears that in the first weeks after birth, reasons for cessation are mostly related to physiology (Vogel et al., 2009, p.37-39; Bulk-Bunschoten et al., 2008; TNO, 2015). Furthermore, some reasons for cessation are related to the autonomy of women. For example, several studies found that breastfeeding is experienced as a restriction for some women as they cannot leave their child for more than a few hours unless they pump their breast milk (Vogel et al., 2009: 28; Bulk-Bunschoten et al., 2008). While pain remains a consistent reason for cessation, between the second and fourth month work and time become more central factors (TNO, 2015).
Breastfeeding at work
Between 2002 and 2011, the Netherlands experienced a 2.5 percent increase in the labour force which was completely due to women (Centraal Bureau voor de Statistiek, 2012). The percentage of Dutch women working for more than 12 hours per week increased from 53 percent in 2002 to 60 percent in 2011 (Centraal Bureau voor de Statistiek, 2012). In 2007, the Netherlands renewed its labour laws concerning pregnancy and breastfeeding. These laws allow women to take up to 16 weeks of leave, comprising a 6-week pregnancy leave and a 10-week maternity leave (Rijksoverheid, n.d.). Furthermore, these laws state that employers are obliged to provide a suitable space and extra work breaks (up to 25 percent of their work time) on request for breastfeeding women until their child is 9 months old (The Working Hours Act, Article 4:8, paragraph 2). Considering that work is a main reason to stop breastfeeding, this raises the question of the degree to which these laws are followed (The Working Hours Act, Article 4:8, paragraph 2).
Normalising judgement
Furthermore, although not emphasised, a recurrent theme in a study by Vogel et al. (2009) is the influence of a mother’s social environment on her breastfeeding practices. Besides unco-operative employers, being sent away from public places is another example of negative attitudes towards breastfeeding. Some women explained that they would feel less restricted by breastfeeding if it were socially acceptable to breastfeed in public (Vogel et al., 2009: 29). Indeed, a study commissioned by Voedingscentrum (2010) found that breastfeeding in public is considered ‘abnormal’ by 45 percent of Dutch people. According to Foucault (1975), ‘normalising judgement’ stems from societal norms and is a form of disciplinary power which is used to punish abnormal behaviour. It is argued to be fundamental to the modern ‘disciplinary’ society (Foucault, 1975). Studies found that normalising judgement with regard to breastfeeding in public appears in the form of recalcitrant attitudes, discouraging looks and harassing comments towards breastfeeding women (Cox et al., 2007; Khoday and Srinivasan, 2013; Tsai, 2013; Vogel et al., 2009).
Changing norms
Normalising judgement can be understood as a reaction to change in breastfeeding practices. Breastfeeding patterns appear to be cyclic. In the Netherlands there was an increase in breastfeeding rates between the 1850s and the 1920s due to progressive understanding of associated health benefits (Thorvaldsen, 2008). This was followed by a rapid decrease due to World War II as a result of stress and malnutrition among mothers (Thorvaldsen, 2008). Although breastfeeding rates increased after World War II, in the 1960s breastfeeding rates were especially low (Thorvaldsen, 2008). This can be explained by the rise of feminism and women’s increasing desire for autonomy. In addition, developments in scientific research and medical practice created the notion of ‘scientific motherhood’: women had to rely on expert knowledge regarding childbearing advise (Martucci, 2011). At the same time, the increase in infant food manufacturing and its modern and scientific connotation increased the use of formula feeding (Martucci, 2011). Bottle-feeding allowed for the greater inclusion of the father in family life. As a result, scientific motherhood became embedded in healthcare structures and changed maternal expectations (Martucci, 2011). However, a different ideology regarding motherhood emerged in the 198’s; ‘natural motherhood’. Here, the emphasis is on following maternal instincts, breastfeeding, and less on the medicalisation of child rearing (Martucci, 2011). The technological invention of the breastmilk pump allowed natural motherhood while still retaining autonomy and including the father in the child-feeding process. This subsequently caused a rise in breastfeeding rates.
Body perception
In addition, some studies suggest that prevailing norms and ideologies concerning the female body are likely to have an influence on women’s breastfeeding behaviour (Cox et al., 2007; Khoday and Srinivasan, 2013). Breasts are often associated with sexuality rather than their biological function – that is, nursing infants (Johnston-Robledo et al., 2007). Theories suggest that breastfeeding reminds others of the ‘physical, animal nature of humanity’, which is a reminder of the unalterable mortality of people; or that breastfeeding and pregnancy corresponds with having a ‘good maternal body’ (Cox et al., 2007; Johnston-Robledo et al., 2007). According to the objectification theory, women are inclined to view themselves from the perspective of an outsider due to objectification of their bodies (Frederickson and Roberts, 1997). Thus, if breastfeeding is not considered ‘sexy’, and is even viewed as visually unappealing by some, women may feel pressured to discontinue breastfeeding to feel sexually attractive again (Johnston-Robledo et al., 2007).
Since there is a lack of literature on the influence of societal norms on breastfeeding, this study addresses the following research question: how do norms and ideologies – both personal and societal – influence the breastfeeding experiences and practices of Dutch women? A greater understanding of these barriers will allow for more targeted campaigns or interventions to improve breastfeeding rates.
Methodology
Setting
The Netherlands is ranked among the countries with the best healthcare systems in the world (Björnberg, 2015). It has a unique system of public health monitoring which uses so-called ‘consultatiebureaus’, or youth care centres (JGZ)[1], to assess children’s health status and to advise mothers from all social classes about child nutrition, infant feeding and hygiene (Beer, 2004). Furthermore, breastfeeding rates have remained low despite information provided by organisations like Platform Borstvoeding[2], laws to promote breastfeeding at the workplace, and healthcare being widely available. This makes the Netherlands an especially interesting subject for a case study.
Study design
A mixed-methods approach consisting of in-depth interviews, one focus-group discussion, and a survey informed by these qualitative data was selected as the optimal methodology to generate consensus themes and to explore which factors were shared within a larger population. Convenience sampling was used for the interviews and is herein defined. To be included in the study, women had to hold Dutch nationality and had to be currently breastfeeding, or have breastfed in the last 10 years. The timeframe of 10 years was chosen based on the renewing of the Dutch Working Hour act in 2007 and this was deemed an appropriate time period to reflect contemporary life. For the survey, voluntary sampling was used. The survey was distributed via Facebook; hence, the sample is made up of self-selected women. The inclusion criteria for the survey were that the respondents were women with breastfeeding experience.
Data collection and procedure
Mothers were recruited via JongFlorence (the youth health centre in The Hague) using recruitment leaflets and via a contact person from the Mamma café.[3] Emails were sent to multiple organisations affiliated with breastfeeding. The survey was created via www.surveymonkey.nl, and was distributed via social media.[4] The survey consisted of 30 questions in total, of which some were general background questions, such as age and number of children. The remaining questions were specific to the subtopics of breastfeeding, such as work, public breastfeeding and pumping milk. A variety of question types were used: Likert scale ranking, open-ended questions and multiple choice. Moreover, per subtopic, the option was given to provide further explanation for contextualisation.
Data analysis
Core themes in the interview data were analysed using an inductive thematic approach. This method of analysing qualitative data results in an exhaustive and rich account of a larger body of data (Braun and Clarke, 2006). All transcripts were reviewed and coded systematically based on the interview guidelines. The individual data extracts were combined and read line by line to identify recurrent themes and concepts. The identified themes were: efforts made by mothers, ‘good’ motherhood, social support and lack thereof, institutional barriers, concealment, regaining autonomy and normativity. In the third round of coding, connections were made between themes within the different interview topics.
The initial survey was slightly altered based on feedback from participants. The results of the surveys were imported into a spreadsheet to calculate descriptive statistics and create graphs.
Results and discussion
Participants
In total, 12 interviews were conducted with mothers via Skype, in person and over the phone, lasting about 45 minutes each. Two of the nine organisations responded for the expert interviews: an employee at one of the Dutch youth health centres (JGZ hereafter) in The Hague, and Karen van Drongelen, the co-ordinator of Platform Borstvoeding. The interviews were held at the respondents’ places of work. Moreover, one Mamma café of approximately three hours was attended which functioned as an informal focus-group discussion; four new mothers, one lactation consultant and one midwife were present. The discussion was not recorded due to ethical considerations; however, notes were made and permission was sought to ensure certain information could be used in this research. All in-depth interviews were performed in Dutch, audio recorded and transcribed in Dutch. Specific quotations were translated into English by the researcher. One interview was omitted from the research as the audio was inaudible due to technical failure.
Characteristics of study population
The age range of the women participating in the interviews was 25 to 39. Eight of the 11 women were currently breastfeeding; one woman was pumping exclusively and two women recently stopped breastfeeding. All but one woman breastfed in the last three years. The duration of breastfeeding ranged from 13 weeks to three years. Five of the women were married, six were in a relationship and one had recently separated from her partner. The characteristics for all interviewees are provided in Table 1. For privacy considerations, all names have been changed in this research. Further, a total of 1160 Dutch women participated in the survey (Figure 1). The mean age of the respondents was 32.62 years (SD=5.07). At the moment of the survey, 47.4 percent of the women was still breastfeeding. The majority had one or two children (43.3 percent and 39.7 percent respectively), 14.0 percent had three children, while 3 percent had four or more children.
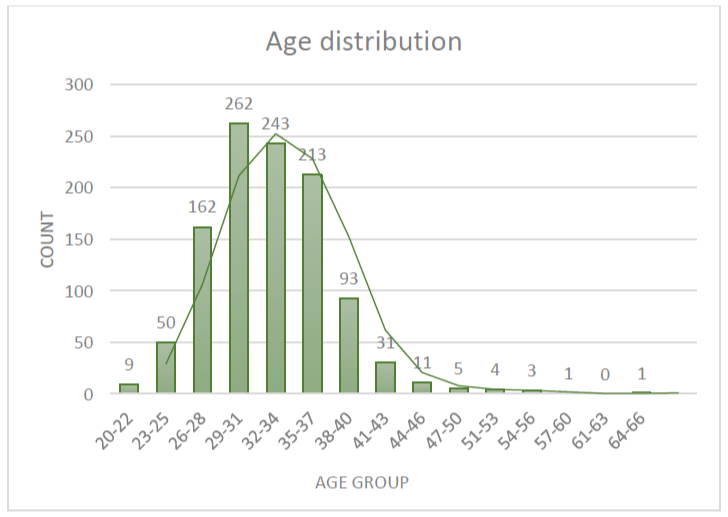
Figure 1: Age distribution (N=1089) based on the survey.
|
# children per interviewee |
Duration of breastfeeding |
Still breastfeeding |
Working |
Place of birth |
Relationship status |
|---|---|---|---|---|---|
|
1 |
24 weeks |
Yes |
Yes |
Home |
In a relationship |
|
1 |
13 weeks |
Yes |
Yes |
Hospital |
In a relationship |
|
2 (twins) |
60 weeks |
No |
Yes |
Hospital |
Married |
|
1 |
12 months |
Yes |
No |
Home |
Married |
|
1 |
6 months |
No |
Yes |
Hospital |
In a relationship |
|
2 |
8 months and 22 months |
Yes, only the youngest |
No |
Hospital |
Separated |
|
2 |
2 years and 5 months; and 3 months |
Yes, both |
Yes |
First one at home, second in hospital |
In a relationship |
|
1 |
7 months |
Pumping milk exclusively |
Yes |
Hospital |
Married |
|
2 |
3 years; and 15 months |
Yes, both |
Yes |
Unknown |
Married |
|
1 |
19 months |
Yes |
Yes |
Hospital |
In a relationship |
|
2 |
3 months and 10 months |
Yes, only the youngest |
No |
Both at home |
Married |
Table 1: Characteristics of the interview participants.
Survey results: Motherhood
It is an investment, but it is definitely worth the investment. In the sense of time and energy, and definitely in the beginning also persistence and suffering. I experience the moments of breastfeeding as very pleasant, very intimate. It is also beautiful to know that your child is growing because of what you’re giving to her.
Susie, mother of 19-month-old Ella, captures the essence of the experience with breastfeeding with this quotation. To start or continue breastfeeding is not simply a decision mothers make. The mothers’ stories about persisting despite infections, cracked nipples and fatigue made it clear that breastfeeding is a process with many obstacles and victories. The decision to start breastfeeding and the motivation to continue appear to arise partly from the feeling that it is the logical decision for a mother to make. Susie elaborated:
My motivation at that time was – see, to me, breastfeeding is in line with how I live. It just lines up completely with how I see the world and how everything works.
This is in the sense that it feels like the right decision to make for a mother, not that it is the easiest decision to make. A great part of this is determined by a mother’s perception of what is healthy. Breastfeeding is often see as the best thing a mother could possibly do for her child. Anne, for example, said:
Because I just really wanted to, and I am convinced that breastmilk is the best thing there is for a baby. […] I really think it’s simply the best there is. All mothers produce their own milk, specifically for their own baby. Nutricia[5] can’t make it that well, because they produce it for all babies.
Perhaps the clearest distinction made here is that breastmilk is considered to be natural, while a commercial, generic product such as formula feeding is seen as unnatural. This creates a dichotomy between the two: natural versus unnatural, healthy versus unhealthy, natural versus scientific motherhood.
Institutional barriers in healthcare provision
Opposing ideologies concerning motherhood can cause clashes with healthcare provision since the principles of scientific motherhood are still embedded in care structures. For example, Melissa noted:
There is of course a whole generation brought up with bottle-feeding, and Nutricia has close ties with the JGZ, you notice that about everything.
Karen van Drongelen agreed that the ideologies of healthcare providers play a role in this as most of the healthcare providers were raised during the 1960s and 1970s, during which scientific motherhood prevailed. For this ‘bottle-feeding generation’ formula feeding may be seen as normal and they may form their advice accordingly. With regard to Nutricia’s covert marketing strategies, she explained:
The fact of the matter is that physicians, and healthcare providers as well, are approached by manufacturers with information about their products. And well, I wonder how objective that all is. They do attempt everything, you see, they give all sorts of gifts. Or even just a pen; they did a lot of studies on that, the effect of holding something every day – because there is a name brand on that, you do unwittingly register that in your mind […] what kind of double message are you giving that way?
Another clear example of a stumbling block at the JGZ is when babies are measured and weighed. Kacey explained:
I find that annoying about the JGZ, that the weight and growth is compared to the curve of an infant with formula feeding, while everybody knows that breastmilk is much better for the child, and that curve is completely different.
Negative experiences with the JGZ were clearly reflected in the survey: approximately one third of 845 women thought that the care from the JGZ was either bad or very bad, while 36.3 percent had a neutral stance on this; only 17.4 percent thought the care was either good or very good (see Table 2).
| Very good | Good | Neutral | Bad | Very bad | N/A | Total N | |
|---|---|---|---|---|---|---|---|
| Lactation consultant (N) | 219 | 219 | 56 | 21 | 5 | 312 | 832 |
| 26.32% | 26.32% | 6.73% | 2.52% | 0.60% | 37.50% | ||
| Maternity care provider (N) | 241 | 379 | 120 | 64 | 14 | 48 | 866 |
| 27.83% | 43.76% | 13.86% | 7.39% | 1.62% | 5.54% | ||
| JGZ (N) | 21 | 126 | 307 | 209 | 58 | 124 | 845 |
| 2.49% | 14.91% | 36.33% | 24.73% | 6.86% | 14.67% | ||
| Breastfeeding café (N) | 43 | 71 | 63 | 9 | 7 | 584 | 777 |
| 5.53% | 9.14% | 8.11% | 1.16% | 0.90% | 75.16% | ||
| Midwife (N) | 139 | 305 | 210 | 42 | 8 | 143 | 847 |
| 16.41% | 36.01% | 24.79% | 4.96% | 0.94% | 16.88% | ||
| Hospital (N) | 82 | 233 | 187 | 173 | 56 | 123 | 854 |
| 9.60% | 27.28% | 21.90% | 20.26% | 6.56% | 14.40% |
Table 2: Experience with care providers.
Furthermore, Susie stated:
What I thought, and this is nice to connect to what we were discussing about the mamma café; they have a starting time, but they say: ‘It doesn’t matter when you walk in, we’re just going to start, we’ll be here, just see for yourself’. I find that fantastic. Because that fits exactly with the way of life of a breastfeeding or a new mother.
This quotation refers to the appointments set at a specific time at the JGZ, something which was found to be of hindrance since the life of a new mother is rather unpredictable, as a baby can suddenly request to drink or need a clean nappy.
Not only is the quality of care provision a concern, the quantity is as well. Maternity care is provided for up to eight days after birth, yet the first meeting at the JGZ is at one month after birth. Karen van Drongelen explained how this contributes to why most women quit breastfeeding during the first two weeks:
They end up in a black hole; if things go differently than expected or it hurts, or – well there can be numerous reasons, the threshold to say ‘it’s because of the breastfeeding and I quit’ – is just very low.
Thus, women face institutional barriers as well: guidance from healthcare providers is lacking. Although maternity care is generally greatly appreciated, physical problems often arise after the first week and women indicated that they needed extra guidance and support. As a result, it is precisely during this gap between healthcare provision that we find the largest proportion of women discontinuing breastfeeding. This is especially interesting since the Netherlands is known for its unique system of public health monitoring and healthcare provision for new mothers. It is true that additional guidance at, for example, breastfeeding cafes is available for women who face difficulties; lactation consultants in particular were deemed to be of tremendous benefit. However, this extra help is not necessarily covered by insurance companies and mothers have to take the initiative to find suitable guidance themselves. For some women, this is yet another barrier to continuing breastfeeding when they are already experiencing setbacks.
Institutional barriers in the workplace
Institutional barriers are noticeable in the workplace as well. Since employers have their own ideas about breastfeeding, this can shape their willingness to providing lactation space and time. Only approximately one third of all employers had a positive attitude towards pumping milk at work (see Figure 2). Moreover, Julia and Emma gave examples of comments women may have to endure:
Well, because my employer said to me during my pregnancy: ‘You’re not going to breastfeed, right? Oh, gross, I think that’s nasty.’
My employer was like: just quit [breastfeeding] already. But that was purely out of his own interest. Because, if I don’t pump milk, I am more employable for my boss.
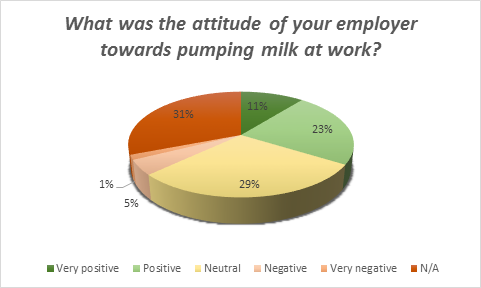
Figure 2: Attitude of employers towards pumping milk at work (N=955).
The existing laws pertaining to breastfeeding in the workplace appear to be ignored. Two thirds of all the women indicated that they had struggled in some way with finding access to an appropriate lactation space (see Figure 3). This sometimes resulted in them having to pump milk in improvised spaces, such as bathrooms, kitchens and even broom closets and toilets.
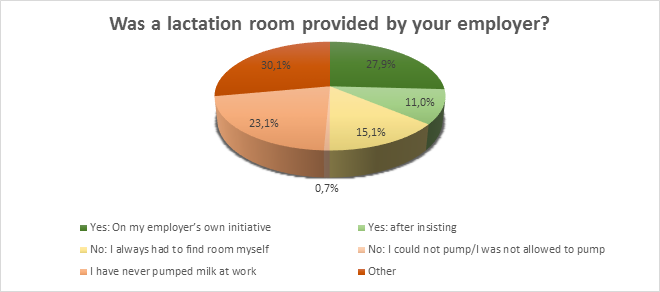
Figure 3: Provision of lactation space (N=926).
Furthermore, the attitudes of colleagues can greatly affect how comfortable a woman is pumping milk at work as well. Rian stated:
They do tell you: ‘Your colleagues will need to fill in for you.’ That makes you feel bad for your colleagues. And it also feels like discouragement, right, passive aggressive. Because they had a negative attitude towards it and found it troublesome, I did not want to, you know, trouble them again. When I said I was going to pump milk; they would sigh agitatedly.
As this indicates, a generally unco-operative attitude from both employer and colleagues can create feelings of guilt and cause stress. Not being able to pump milk can cause pain, breast infections and even cause the milk production to decrease. Therefore, sub-optimal arrangements for pumping milk at work are for many women a reason to discontinue breastfeeding. A possible explanation for the negative attitudes of some employers and colleagues, as reviewed in the introduction, could be that the current workforce stems in large part from the ‘bottle-feeding generation’. Another possible explanation is that women have increasingly become part of the workforce in recent years and laws were only changed in 2007; pumping milk at work is thus a novelty to a certain extent. This consequently may challenge pre-existing norms of the workplace.
Normativity
Contrary to what was expected, changing body image and societal pressure and expectations of the female body regarding sexuality did not appear to influence women’s breastfeeding experiences and practices. The duration of breastfeeding appeared to generate most societal pressure: breastfeeding a toddler was found to be a foreign or even uncomfortable image. For example, Rian still feeds her 3-year-old daughter and stated:
There’s no one – almost no one, of my close friends – who know that she still gets some breastmilk from me in the evening […] It is definitely a taboo, very clearly. Because it’s just not done, since she can already speak […] I did tell someone a while ago, and they stared at me like, ‘What planet do you come from?! We don’t live in a Third World country where they advise you to breastfeed until 2.5 years.’
Interestingly, the woman Rian disclosed this to associated breastfeeding toddlers with something which is done in Third World countries. This is a clear example of how certain images people have about breastfeeding determine what they find normal practices. In addition, Susie stated:
A baby gets breastmilk, and that is until approximately 6 months. After that, I did notice I got more comments along the lines of ‘Oh, are you still breastfeeding?’. Not negative per se, but they were notable.
This conception that feeding a child older than approximately 6 months deviates from the norm is noticeable from other comments as well. For example, when asked about positive responses from her social environment, Susie responded:
Some, well I think that most women think it’s good of me, or great, that’s what I heard a lot: ‘So great you’re breastfeeding’, or ‘Well done, you’re still breastfeeding’.
Although these are positive and supportive comments, the word ‘still’ simultaneously indicates that these women find it special that Susie still feeds her 19-month-old daughter. According to Karen van Drongelen (JGZ), being afraid to be associated with breastfeeding fanatics is a real concern:
See, in the Netherlands it is not so common [to breastfeed for a long time]. And the women who do feed for so long are usually the types that expose everything and think that should all just be okay. And that just doesn’t help, I think that women who do breastfeed do not want to be associated with that. […] when you know that already so many women feed for such a short time, that is actually just – it just detracts. It scares them off.
Thus, feeding a toddler may have a negative connotations, as it is associated with the ‘breastfeeding mafia’; women who feed their child very demonstratively. Hence, although some women would feed their toddler at home, they were more reluctant to feed their child in a public setting.
I notice that now, with my daughter, I do in fact want to start phasing out. I’m thinking, you’re almost 2.5 years old now, it’s kind of done now […] If I imagine I would still be feeding her when she is 4, I don’t think it would be appropriate. I think it has to do with that we are raised with the thought that breastmilk is for babies, and the older she gets, the more I get the feeling that she is getting too old for it.
As this quotation from Melanie shows, normative ideas are decisive in when a mother finds it appropriate to start phasing out or to stop breastfeeding.
Concealment
A woman’s decision not to tell others she is ‘still’ breastfeeding is one form of concealment. A second form is physically concealing the act of breastfeeding. Ida, for example, said:
I am aware of the people around me. So, I do check what they think of it, or I will look for a quiet place so I am not standing in the way of anyone. Because I am aware that not everyone might find it appropriate […] When I breastfed on the train, I purposely sat in a two-sits, not those with four people, so to speak, with people sitting across of you. And I think I also covered up with a scarf.
From this quotation, it becomes clear that women are aware of the fact that breastfeeding is not normalised in the Netherlands, and they adjust their practices accordingly. Women often use specific clothing such as breastfeeding bras and breastfeeding t-shirts.
I do it [breastfeeding] a bit below my shirt. I do often think, if you’re still going to complain that I am breastfeeding, you really must have tried to see it.
As Melanie illustrates by this statement, women conceal that they are breastfeeding because other people might find it abnormal or socially unacceptable. Public breastfeeding was sometimes experienced as uncomfortable regardless of the infant’s age, which reinforces the position of Lock and Nguyen (2010) that social context can influence embodied experiences. This illustrates how societal norms can shape a woman’s breastfeeding behaviour. Nevertheless, the majority of women indicated that they had breastfed in public (see Figure 4). Table 3 provides additional reasons for why some women choose not to breastfeed in public.
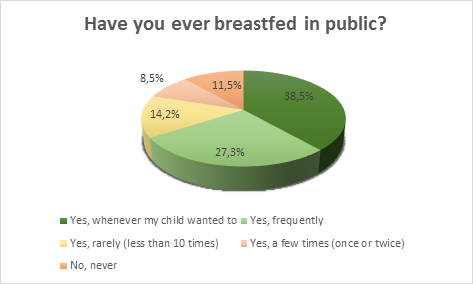
Figure 4: Public breastfeeding (N=1032).
Interestingly, it appears that normalising judgement and stigmatisation of breastfeeding in public is not as great a concern as expected, despite the finding that 45 percent of Dutch people find it abnormal when women breastfeed in public. An explanation could be that since women breastfeed relatively discreetly and take their surroundings into consideration, people do not take offence, do not dare to comment, or simply do not notice. It should be noted that it appeared from the in-depth interviews that the definition of public breastfeeding can be very broad. Some women interpreted this as feeding in their car, or in a private room at a public place. This means that the number of women who breastfeed in sight of other people is lower. Another explanation could be that people imagine public breastfeeding differently; perhaps the 45 percent indicating that they find it abnormal envision a woman completely revealed, while in practice this rarely happens.
| Why have you never or rarely breastfed in public? | Average response percentage | N |
|---|---|---|
| Situation has never occurred | 37.6% | 163 |
| I find it unpleasant people might see my breasts | 21.0% | 89 |
| I am afraid people will take offence | 14.0% | 56 |
| My partner does not want me to | 1.3% | 8 |
| I feel vulnerable while breastfeeding | 17.4% | 76 |
| Religious reasons | 0.8% | 4 |
| I think it is inappropriate | 5.5% | 25 |
| Other | 3.8% | 19 |
| Other. further explanation | 34.8% | 142 |
Table 3: Reasons for not feeding in public (N=429).
Lastly, and unexpectedly, Platform Borstvoeding is not actively campaigning to normalise breastfeeding:
We made it an element of ordinary infant nutrition [in their magazine], so that you don’t put it on a pedestal. On the one hand, this might be necessary to put it on the agenda more, but on the other hand, it creates the feeling that it is something extra that women can do. And what we want is that breastfeeding becomes self-evident, that is it normal and ordinary. That it is the norm. Momentarily, that is often bottle-feeding or formula feeding, which is seen as normal, while breastmilk is seen as something additional. Even though, say, that should be precisely the other way around.
Limitations to the research
One limitation of this research is that the data is centred on women, thereby excluding the perspective of their partners, employers and social environment. Thus, statements made concerning their ideologies are based on assumptions and from the perspective of the mothers, rather than being based on personal accounts. Furthermore, despite the fact that this research was carefully prepared, and data collection and analysis were done rigorously, some limitations of the data collection require attention. First of all, the questions and definitions in the survey may have been interpreted differently by the respondents. Secondly, some women indicated that they found certain questions difficult to answer. For example, ‘did you give birth in the hospital or at home?’ was unanswerable for multiparous women. Thirdly, women could not be excluded from participating in the survey, therefore it was not possible to set the timeframe of 10 years and to include only Dutch women. However, since the survey was posted in mother groups on Facebook, it is likely that most respondents were women who fit the first criterion. The second criterion may be a cause for bias. Moreover, since the survey was posted in pro-breastfeeding groups (but also in general mother groups) it is likely that women with a strong affiliation with breastfeeding participated. Lastly, only two expert interviews were held due to a low response rate, which limits the professional and policy perspective.
Conclusion
To conclude, early breastfeeding cessation is a public health concern for women and children in the Netherlands. Since breastfeeding can protect both mother and child from various short-term and long-term diseases, it is highly desirable that the guidelines of the WHO are followed. Norms and ideologies, both personal and societal, underlie many of the reasons why women decide to stop breastfeeding. Contemporary mothers seem to prefer breastmilk over formula feeding. This shift from scientific motherhood to natural motherhood appears to be a cause for resistance from society since formula feeding is still the norm for many people. This becomes clear from institutional barriers such as growth curves based on formula feeding at the JGZ, and a lack of suitable lactation spaces at work. It seems that breastfeeding is ‘normal’ as long as the baby is up to six months old and the breasts are covered up. Any practices that deviate from this may evoke a negative response. It is therefore that women decide to conceal themselves when they breastfeed an older infant, and conceal their breasts with special clothing or scarfs, or by repositioning themselves when they are in public. This explains why in previous studies women indicated that they felt restricted by breastfeeding. Women are put in a stressful position in which they have to choose between what is best for their child and what others expect from them as a member of contemporary society. Women are expected to be good employees by being available and not taking time to pump milk, and to be respectful of others by not revealing their breasts in public. However, at the same time women want to be good mothers by providing their child with natural breastmilk. Therefore, normalising breastfeeding in any setting – and up to any age – is not only necessary to improve breastfeeding rates, it is also necessary to relieve this burden that is placed on contemporary mothers.
The findings from this study on how to normalise breastfeeding suggest the need for further research. This should be done for the general population, and more specifically with regard to healthcare provision and pumping milk at work. The role of pharmaceutical companies in the normativity of formula milk could be incorporated in this research as well. Furthermore, additional research could inform more targeted approaches to resolve institutional barriers, for example by replacing the growth curve at the JGZ and adding extra consultations between the last day of maternity care and first appointment of the JGZ. Since the lack of a lactation space in the workplace appears to be a widespread problem, labour groups may wish to get involved.
Acknowledgements
I would like to express my gratitude to my supervisor Josien de Klerk for all her guidance. This artice would not have been made possible without her encouragement, patience and full support.
I am grateful to Elaine and Annemieke for helping me find interview participants. I am also grateful to Karen van Drongelen and all other participants for sharing their experiences with me.
List of figures
Figure 1: Age distribution.
Figure 2: Attitude of employers towards pumping milk at work.
Figure 3: Provision of lactation space.
Figure 4: Public breastfeeding.
List of tables
Table 1: Characteristics of interview participants.
Table 2: Experience with care providers.
Table 3: Reasons for not feeding in public.
Appendix A: Interview guidelines in Dutch
- Hoe lang geeft u al borstvoeding?
- Leeftijd baby, eigen leeftijd.
- Wat is uw fysieke ervaring met borstvoeding geven?
- Hoe heeft u de hulp die u geboden is ervaren?
- Thuis
- Ziekenhuis
- Consultatiebureau
- Heeft u zich van tevoren voorbereid op borstvoeding geven?
- Hoe is het borstvoeding geven verlopen toen u weer ging werken?
- Kolven
- Kolfruimte aangeboden?
- Hoe stond uw werkgever ertegenover?
- Hoe stonden uw collega’s ertegenover?
- Hoe stond uw directe omgeving tegenover het borstvoeding geven?
- Partner
- Familie
- Vrienden
- Heeft u weleens in het openbaar borstvoeding gegeven?
- Op welke manier?
- Heeft u ooit opmerkingen gekregen?
- Is uw lichaamsbeeld veranderd door borstvoeding geven?
- Hoe zou u de gehele ervaring met borstvoeding geven omschrijven?
- Nog ervaringen die u wilt delen?
- Nog vragen?
Appendix B: Interview guidelines in English
- How long have you been breastfeeding?
- Age of baby, own age.
- What is your physical experience with breastfeeding?
- How did you experience the care that was provided?
- At home
- At the hospital
- At the JGZ
- Did you prepare for breastfeeding beforehand?
- How did breastfeeding proceed when you returned to work?
- Pumping milk
- Lactation space provided?
- What was the attitude of your employer?
- What was the attitude of your colleagues?
- What was the view of your direct social circle on breastfeeding?
- Partner
- Family
- Friends
- Have you ever breastfed in public?
- In what way?
- Have you ever received any comments?
- Did your body image change due to breastfeeding?
- How would you describe the overall experience with breastfeeding?
- Do you have any experiences you would like to share?
- Do you have any questions?
Appendix C: Survey
Notes
[1] The JGZ, ‘consultatiebureau’ in Dutch, is a clinic that informs and guides mothers until their child reaches the age of 4. Here, information is provided to mothers on various topics, including breastfeeding. Depending on the municipality, the term consultatiebureau or JGZ is used. For the ease of this research, JGZ will be used.
[2] The campaigns of Platform Borstvoeding are mainly aimed at educating parents and parents-to-be. For example, brochures and information sheets are provided for healthcare providers and other interested people, and briefings are organised. In addition, they also provide guidelines for care providers with regard to breastfeeding.
[3] Mamma cafes are a place where young mothers gather for support on breastfeeding or motherhood.
[4] The weblink was posted in specific Facebook groups for mothers and breastfeeding mothers. The survey link was also posted on the website of https://www.borstvoeding.com/, and was tweeted by and posted on the Facebook page of a blogger. The blogger, who blogs on breastfeeding, and borstvoeding.com were both reached via Facebook.
[5] A manufacturer of formula milk.
References
Allen, J. and D. Hector (2005), ‘Benefits of Breastfeeding’, NSW Public Health Bulletin, 16 (3–4), 42–46
Beer, H. (2015), ‘Observations on the History of Dutch Physical Stature from the Late Middle Ages to the Present’, Economics and Human Biology, 2 (1), 45–55
Björnberg, A. (2015), ‘Euro Health Consumer Index’ (1st ed., p. 4). Health Consumer Powerhouse, available at http://www.healthpowerhouse.com/ files/EHCI_2014/EHCI_2014_report.pdf, accessed 11 April 2016
Braun, V. and V. Clarke (2006), ‘Using thematic analysis in psychology’, Qualitative Research in Psychology, 3 (2), 77–101
Bulk-Bunschoten, A. M. W., P. C. M. Pasker-de Jong, J. P. Van Wouwe and C. J. De Groot (2008), ‘Ethnic Variation in Infant-Feeding Practices in the Netherlands and Weight Gain at 4 Months’, Journal of Human Lactation, 24 (1), 42–49
Centraal Bureau voor de Statistiek (2012), ‘Meer vrouwen aan het werk: vooral in deeltijd?’, available at http://www.cbs.nl/nl/menu/themas/arbeid-sociale zekerheid/publicaties/artikelen/archief/2012/2012-3580wm.htm, accessed 11 April 2016
Cox, C. R., J. L. Goldenberg, J. Arndt and T. Psyzczyncki (2007), ‘Mother's Milk: An Existential Perspective on Negative Reactions to Breast-Feeding’ Pers Soc Psychol Bull, 33 (1), 110–122
Foucault, M. (1977), Discipline and Punish: The Birth of the Prison, trans. A. Sheridan, New York: Vintage Books
Frederickson, B. L and T. Roberts (1997), ‘Objectification Theory: Towards Understanding Women’s Lived Experiences and Mental Health Risks’, Psychology of Women, 21 (2), 173–206
Johnston-Robledo, I., W. Wares, J. Fricker and L. Pasek (2007), ‘Indecent Exposure: Self Objectification and Young Women’s Attitudes Toward Breastfeeding’, Sex Roles, 56 (7), 429–37
Khoday, A. and A. Srinivasan (2013), ‘Reclaiming the Public Space: Breastfeeding Rights, Protection, and Social Attitudes’, McGill Journal of Law and Health, 7 (2), 147–68
Lock, M., and V. K. Nguyen (2010), An Anthropology of Biomedicine, Chicester: Wiley Blackwell
Martucci, J. (2011), ‘Feeding Babies, Making Mothers: The Science, Practice and Meaning of Breastfeeding in the Second Half of the 20th Century’, unpublished PhD thesis, University of Pennsylvania
Morse, J. M., M. Barrett, M. Mayan, K. Olson and J. Spiers (2002), ‘Verification Strategies for Establishing Reliability and Validity in Qualitative Research’, International Journal of Qualitative Methods, 1 (2), 13–22
OECD (2009), ‘Breastfeeding Rates’, available at https://www.oecd.org/els/family/43136964.pdf, accessed 20 February 2016
Thorvaldsen, G. (2008), ‘Was There a European Breastfeeding Pattern?’, History of the Family, 13 (3), 283–95
TNO (2015), ‘Peiling melkvoeding van zuigelingen 2015’, available at https://www.tno.nl/media/5248/peiling-melkvoeding-van-zuigelingen-2015.pdf, accessed 10 February 2016
Tsai, S. Y. (2013). ‘Impact of Breastfeeding-friendly Workplace on an Employed Mother’s Intention to Continue Breastfeeding after Returning to Work’, Breastfeed Med, 8 (2), 210–16
Voedingscentrum (2010), ‘Steeds meer gemeenten borstvoedingsvriendelijk’, available at http://www.voedingscentrum.nl/nl/pers/persberichten/steeds-meer _ gemeentenborstvoedingsvriendelijk.aspx, accessed 10 February 2016
Vogel, I., L. van Rossem, K. van Drongelen, H. H. Haisma, I. Mesters, J. P. van Wouwe and H. Raat (2009), Borstvoeding in de eerste zes maanden, Rotterdam, Instituut Maatschappelijke Gezondheidszorg
Working Hour Act (2015), ‘Arbeidstijdenwet Article 4:8, paragraph 2’, available at http://www.wetboekonline.nl/wet/Arbeidstijdenwet/4.html, accessed 10 February 2016
World Health Organisation (2015), ‘Infant and Young Child Feeding’, available at http://www.who.int/mediacentre/factsheets/fs342/en/, accessed 12 February 2016
To cite this paper please use the following details: van der Zee, M.H.L. (2017), 'Breastfeeding Norms in Contemporary Society: A Case Study of Dutch Women', Reinvention: an International Journal of Undergraduate Research, Volume 10 Issue 2: Featuring the Eramus+ BLASTER Project, https://warwick.ac.uk/fac/cross_fac/iatl/reinvention/archive/volume10issue2/blaster/van-der-zee. Date accessed [insert date]. If you cite this article or use it in any teaching or other related activities please let us know by e-mailing us at Reinventionjournal at warwick dot ac dot uk.