HNA E-Survey Summary
Purpose of the survey
The purpose of this investigation was to identify current practices among prostate cancer teams around England in the assessment of patients’ needs at different stages along the pathway of care. An e-survey (Appendix 1) with a particular focus on the use of holistic needs assessment (HNA) tools was sent out to potential informants in one hundred and forty seven different NHS Acute Trusts.
Method
A key member of the prostate team in each Trust was identified and a first contact was made via telephone either with the team member themselves or with a secretary. With the agreement of the staff member and a confirmation of a relevant email address, the survey link was sent electronically for completion. However gathering data from health professionals has been a difficult task. After an initial mail out to all these contacts, only thirteen online responses were received. A new approach was subsequently adopted and each Trust was telephoned again by a research assistant.
Results
A total of thirty seven submissions have now been made to the online survey. All of these are from different Prostate Cancer Services within NHS Trusts across the country from Sunderland to Cornwall. The locations are shown on the map below (Figure1).
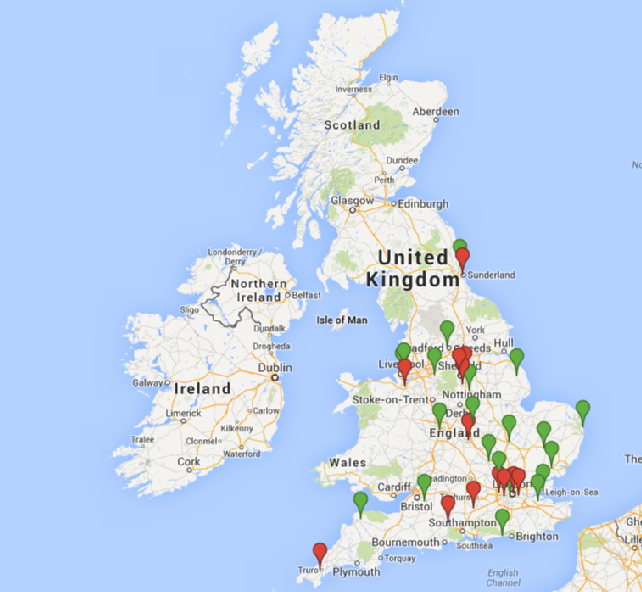
Figure 1 Map of UK showing respondents using and not using HNA instruments (Red indicates trust not using a health needs assessment and green indicates trust using a health needs assessment).
Use of Holistic Needs Assessment Tool
Twenty two services out of the thirty seven are currently using an HNA tool at one or more time point during the care pathway. Seven of the twenty two use a tool only following diagnosis. Other time points at which a tool was used were, post treatment (8 Trusts), post clinical review (3 Trusts), during follow up (7 Trusts), triggered by significant events (7 Trusts) and on transfer to palliative care (7 Trusts). Numbers of time points ranged from 1-6, with 4 Trusts identifying 5 or more possible time points.
Among those services where a tool is not currently in use, eleven use informal assessment. Of these eleven, 6 respondents considered it ‘’too time consuming’’, others mentioned HNA as not being part of standard care and two services described it as ‘’not useful’.
Reasons for not implementing HNA were further explained:
‘I have nowhere to onward refer patients for psychological support if problems are identified.’
Trust 33
‘Difficult to implement with lack of backing from medical staff and lack of resources’
Trust 1
‘One CNS to cover all urological cancers and therefore not sustainable due to number of patients in clinic.’
Trust 18
‘We tried the SPARC tool with 100 patients and asked them what they thought. They didn’t rate it. We just talk to them now!’
Trust 25
Of the twenty two Prostate Cancer Services that currently use an HNA, twenty of these complete the HNA on paper and 2 remotely via telephone. In 5 services the HNA is completed by the nurse only, in 1 by the patient only and in all remaining services a combination of nurse, patient and clinician together. In all cases the HNA is seen by the CNS and in 9 of these services it is further seen by a consultant or other health care professional. In 12 services the patient receives a copy of the HNA but in the remainder the patient is not given a copy. Fifteen services store the HNA in the patient’s case notes, others store the HNA in an electronic file, separate paper file or in the CNS office.
Respondents described a range of HNA tools in current use:
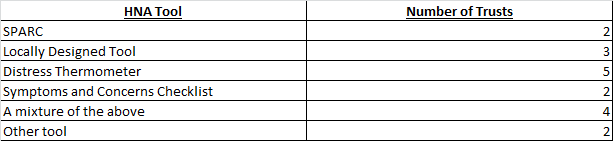
In sixteen Trusts the use of HNA has been adopted as standard practice; in the other 6 Trusts the implementation of HNA was part of service development/innovation.
Evaluation of the HNA has taken place in 2 services (Trust 3 and Trust 12). It is currently being evaluated in 5 services and no evaluation is taking place in fifteen services.
The service development/innovation is currently being evaluated in 5 Trusts and has been evaluated in 1 Trust (Trust 12).
Twenty four services use a risk stratified follow up pathway and eleven do not. Two respondents did not complete this question. Types of follow up for men at low and medium risk are shown in Table 2 below:
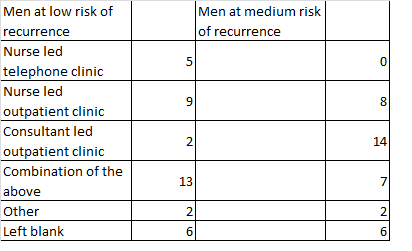
Table 2: Types of follow up in use with men at low and medium risk of recurrence
We asked the question ‘How useful do you think the HNA is to the patient?’:
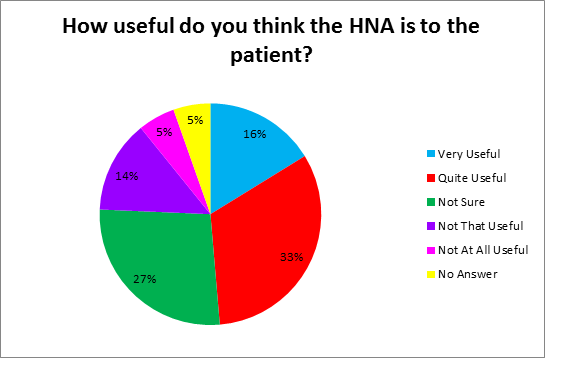
Figure 2: How useful is the HNA to patients?
However it is important to look at the reasons behind these comments. One respondent commented that the HNA was not at useful because,
‘Patients have little desire to fill the forms and they are already freely discussing issues with CNS.’
Trust 32
‘It is only relevant on the day you use it and if you are asking the right questions in clinic you should be able to make a judgement on holistic needs.’
Trust 28
‘I think it is patronising, time consuming and we don’t have the resources to meet the action plan’
Trust 1
Those who were not sure commented:
‘Depends on their relationship with their clinician I think.’
Trust 30
‘the early CAp patients often find the questions very strange considering they are asymptomatic we are telling them they have a potentially curable disease’
Trust 10
The Trusts that found the HNA to be quite useful,
‘Make patients realize their own needs that not necessarily are aware of.’
Trust 29
‘It gives them the opportunity to talk about how they are managing their diagnosis or cancer.’
Trust 23
Those who find the HNA a very useful tool commented:
‘To be able to give a standard record on the discussions about the diagnosis, treatment, useful to have a tool, so everyone knows you have discussed everything. Psychological needs, physical.’
Trust 6
‘Emotional psychological needs and financial needs helps patient but also the family needs (carer's partners)’
Trust 22
In addition some staff made further comments about the use of the HNA. In particular the comments focus on lack of support and time to implement the HNA in current clinical practice.
‘I work with 5 disease sites all of varying disease stages I cover 7 different consultant clinics and 3 nurse led clinics as well as ad hoc clinics and ward patients. I spend so much time trying to fill in and photocopy multiple pieces of required paper that this adds even more! It is doing what I already do but just making it formal. Is anyone auditing patient experience- do they find it beneficial? If so it has to be something all Health care professionals are involved in not just an additional task for CNS's!’
Trust 1
‘It is a challenge to complete the HNA on all patients. It is offered to all patients but not all take the offer up. If they did it would be very difficult to complete with the lack of CNS support available’
Trust 11
‘As a team we are very keen to use HNA's however it is not sustainable currently due to urology capacity for one CNS. We are looking at ways to address this.’
Trust 18
‘Main rationale for using a structured document is due to time - difficult to complete when to do it properly and gain benefit from it, time is required to explore it in detail.’
Trust 37
‘It takes time to complete which wasn't allowed for when introduced into practice. It feels contrived when using it, allows patients to deny problems that more informal discussion and assessment would identify I would like to send it out to patients with their appointment so that they can fill it in and bring it with them, and reduce the time needed to focus on the patient identified issues but have not allowed me to introduce this. The explanation given is that it is meant to be a face to face assessment tool.’
Trust 36
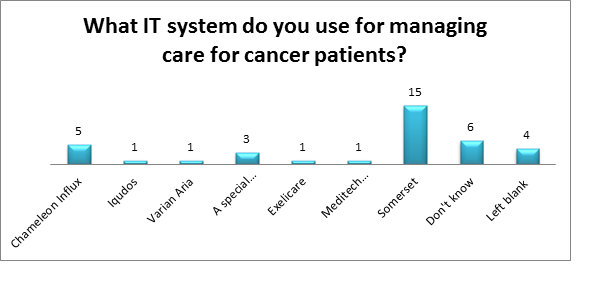
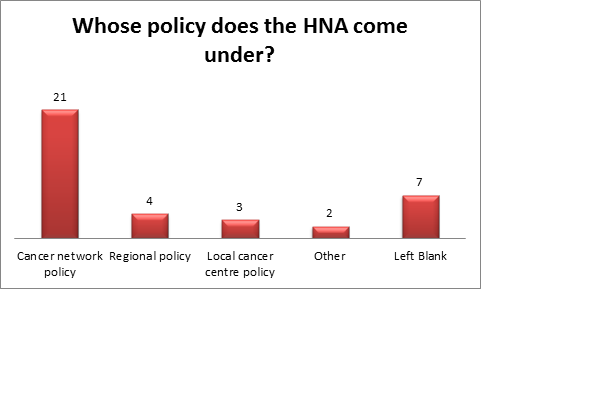
Additional questions related to the IT system in use within the Trust and to the policy context of the use of HNA responses are shown in Figure 3 below:
Limitations
The e-survey was completed by thirty seven respondents from different prostate cancer services within the one hundred and forty seven Acute Trusts in England. All of these Trusts were contacted twice or three times in order to encourage completion of the survey. A staff member from prostate cancer services in two further Trusts contacted the study team without completing the questionnaire. One of these wished to draw attention to the needs of palliative patients and the other to discuss a research idea. The request to complete the e-survey was never refused, however it was apparent that messages were either not passed on or that the survey was not prioritised by busy staff.
Although the e-survey was completed by respondents from only 25% of the prostate cancer services in England, these services were located in Trusts throughout the country as is shown on the map in Figure 1. The relatively similar proportions of services in which HNA tools are used and not used suggest there is no particular bias or overrepresentation of users or non-users. The views of HNA expressed by respondents however should be interpreted with caution as these do not necessarily represent the views of all team members within a particular service.
Conclusion
The data gathered from the e-survey has shown diversity in practice across prostate cancer services. It has also shown divergent views regarding the value of holistic needs assessments. It has highlighted the need to develop an HNA tool that is quick, acceptable and readily integrated into standard practice for all, taking in to consideration the contextual constraints and the views of health care professionals.
