Breaking Barriers in Clinical Communication: Are Securely Attached Doctors More Empathetic Doctors?
by Kirsten Atherton, Anna Chisholm, Lucie Rutter, Sarah Peters, School of Psychological Sciences, University of Manchester and Ian Fletcher, Division of Clinical Psychology, University of Liverpool
ABSTRACT
Patients often present hints to emotional issues in clinical interactions. However, these are often missed by healthcare providers. It is unknown why some healthcare providers attend to more patient cues/concerns than others. Bowlby’s Attachment theory (1973) relates experiences in infancy to adult relationship models and some evidence suggests that attachment relationship models can predict health provider willingness to engage with emotional aspects of patients’ consultations. However it is not known if this association can be demonstrated during medical training, i.e. at a time when educational intervention is feasible. The aim of this study was to examine whether securely attached student doctors respond to patient cues/concerns in a more empathic manner compared to insecurely attached student doctors. Videotaped interactions between student doctors and simulated patients were coded for responses to patient-initiated cues and concerns. These were compared between securely and insecurely attached students. Contrary to our hypothesis there were no significant differences between securely and insecurely attached student doctors. Theoretical and methodological issues are discussed in order to address how to develop this important area of healthcare research.
KEY WORDS: attachment, clinical communication, empathy, healthcare provider, patient.
Introduction
The Chief Medical Officer Sir Liam Donaldson’s proposal of a five-yearly revalidation of doctors’ medical licenses has caused a stir and pushed communication into the forefront of a doctor’s skill base once more. The president of the General Medical Council, Sir Graeme Catto, believes it to be ‘the biggest change to medical regulation in 150 years’ (Boseley, 2008: 1). The plans state that patients will play a key role in the revalidation process by giving feedback about how well their doctor listens to them, shows respect, and how involved they feel in decisions regarding their treatment (Boseley, 2008). Not only does the proposal highlight the importance of doctor-patient communication, it also emphasises the importance of communication within a multidisciplinary team. It is expected that a more cohesive medical team will provide a better standard of care and reduce negative feedback. The plans suggest that a staff member will be appointed to gather information to ensure that ‘five years worth of evidence and testimonials’ (Boseley, 2008: 1) are prepared for each revalidation check. This may be the catalyst for a culture change in the healthcare environment towards a situation where disagreements among doctors and any of the multidisciplinary team results in ‘whistle-blowing’ to the administrative staff (Boseley, 2008).
The importance of doctor communication has been highlighted through Engel’s (1977) biopsychosocial model of illness which provides an alternative to the traditional biomedical model. Previously, it was thought that illness resulted from organic pathology (i.e. disease) and that whilst mood changes may occur when one is ill, psychological factors have no influence on the onset of illness. In contrast, according to Engel (1977), causes of illness include a possible combination of biological, psychological and social influences. The implications for the medical profession are that doctors should not only treat the physical problem but the person as a whole. This presents a challenge for doctors as physical symptoms are often more tangible and evident in a person than psychological problems which can be more difficult to quantify. Doctors must learn to communicate with patients in ways that build mutual understanding in order to detect psychological burdens.
Effective communication between doctors and patients is also crucial as there are multiple objectives for a consultation from both the doctor and patient’s perspective, such as full information gathering; responding to the patient’s needs and concerns; and gaining support or advice. It has been found that the specific goals of doctors and patients are not always congruent and may have slightly different orientations (Nordin et al., 2006). More specifically, goals were similar in that they both aimed to find the cause of illness and improve patients’ functioning and coping. However, doctors were more focused on symptom alleviation while patients rated holistic support from their clinician most highly. This demonstrates that whilst both sides seek a satisfying outcome, the definition of what this involves differs between doctor and patient. However, the key to achieving these outcomes is successful clinical communication.
The relationship between a doctor and a patient is unique, delicate and notoriously complex (Salmon & Young, 2005). Influences include the fact that patients are seeking help from someone they may not know, about issues which they consider highly important and personal and may lead to significant emotional strains. This, coupled with the frequently perceived uneven power ratio between each party, can lead to either side feeling uncomfortable (Ong et al., 1995). It is important to note that some of the most frequent causes of complaints to UK hospital trusts are a result of poor communication (Dacre et al., 2004).
Trust is integral within the doctor-patient relationship and is one of the more influential factors in improving the patient’s outcome from the healthcare interaction (Safran et al.,1998. Cited in Ohtaki et al., 2003). Wittink et al.’s (2006) paper relating to important aspects of care for patients with depression highlights the crucial nature of good communication between the doctor and patient. Patients may question their diagnosis or treatment plan, therefore an attentive and approachable doctor can make a big difference in allowing a patient to be more forthcoming with their concerns (Wittink et al., 2006). Doctors also benefit from an open and empathetic relationship with their patients as more information is made available for the diagnostic process. Doctors who did not engage with patients in this beneficial manner report low satisfaction and an increased rate of ‘burn out’ (Roter et al., 1997). Ultimately, it was concluded that provided the doctor maintained his/her ability to consider a patient’s case objectively, a close empathic relationship should make each stage of the diagnostic and treatment process more fluid and effective (ibid).
As communication is deemed to be an essential skill, researchers have developed methods of teaching communication skills to medical professionals and students around the world. It is the opinion of many researchers that communication skills can be learnt and continually improved upon (Dacre et al., 2004). It is proposed that training in active listening should be implemented widely throughout the health care system, from experienced practising doctors to medical students (Lang et al., 2000). Such training alerts doctors to clues in patient dialogue which may expose information about family histories and prior knowledge of their condition. The Toronto Consensus is a statement created by a group of international experts in the field of communication in healthcare. The statement includes ideas of how skilled communication can help the patient disclose any illness perceptions they may have gained prior to the consultation or diagnosis (Simpson et al., 1991). It is understood that illness perceptions can cause feelings of anxiety, panic and fear in patients, often unnecessarily. Often patients do not express these feelings for reasons such as the assumption that the doctor will know what their concern is and address it automatically, or that the idea is too embarrassing to admit to a trained doctor (Peters et al., 2009).
Unfortunately, there have been reports suggesting that training courses are not always well received by doctors and can be disregarded by some as lacking scientific clout (Simpson et al., 1991). Certain elements of the aforementioned reaction may be due to the fact that a proportion of doctors avoid addressing emotional issues. Doctors often do not feel confident in their ability to respond appropriately to emotional problems because it may ‘open a can of worms’ (Maguire & Pitceathly, 2002). Doctors with this attitude may use behaviours to avoid emotional issues such as not acknowledging the emotional content in a conversation, actively changing the subject or focussing purely on the physical problem. These are the circumstances which lead to only half of patients’ concerns being addressed and more importantly missed cases of psychological morbidity (Griffin et al., 2004; Maguire & Pitceathly, 2002).
It is suggested that a doctor-patient consultation involves a two-stage approach (Ong et al., 1995). One stage is designed to focus on the practical medical complaint; coined as the ‘cure’ system, and the other is designed to focus on the emotional content of the interaction; coined as the ‘care’ system. Ultimately, the ideal consultation would fulfil a patient’s needs in both systems: ‘ the need to know and understand (cure) and the need to feel known and understood (care)’ (Ong et al., 1995: 904). To achieve both of these targets, a doctor must have the ability to attend empathetically to patient emotions displayed within a consultation.
There are various views on how empathy is defined and how it should be used as an effective tool in clinical communication. Perhaps the most widely accepted is captured by The Society for General Internal Medicine, who define empathy as ‘the act of correctly acknowledging the emotional state of another without experiencing the state oneself’ (Halpern, 2003: 670).
Bowlby’s (1973) attachment theory proposed that the experiences within the relationship between a child and their caregiver form cognitive schemas known as ‘internal working models’. These models determine how we act in interpersonal relationships later in life. The advantage if this theory is correct is that a child who has had a very stable childhood with supportive caregivers perceive themselves as ‘worthy of care’ (model of self) and ‘trust others’ (model of others) to provide care (Ciechanowski et al., 2002). The system of attachment has two purposes; the first of which is as a means of protection by maintaining a close proximity to the primary caregiver and the second to utilise the caregiver as a consistent base to explore from when protection is not necessary (Hunter & Maunder, 2001).
Based on Bowlby’s (1973) theory, Bartholomew and Horowitz (1991) developed a classification system for adults - a secure attachment style and three insecure attachment styles; dismissing, preoccupied and fearful. Securely attached adults have experienced continually responsive care giving, creating a positive impression of themselves and other people which consequently makes them at ease in situations involving asking for help or receiving help from others (Ainsworth et al., 1978. Cited in Ciechanowski et al., 2002). Adults with a dismissing attachment style had continually unresponsive caregivers and consequently became instinctively independent (Bowlby, 1977). This creates a positive self-view but they ultimately have a negative view of others and do not easily place trust in other people.
People whose caregivers were inconsistently responsive are more likely to be classified as having a preoccupied attachment status. They have a positive view of others and are emotionally dependant on others for approval. Contrastingly, they have a very negative self-view. Adults who have a fearful attachment style crave social approval and contact. They are, however, ultimately repressed through fear of the expected result: rejection. The caregivers of a fearful person were excessively dismissing or unkind (Bartholomew, 1993. Cited in Ciechanowski et al., 2002).
Research suggests that attachment status influences patient behaviour within clinical settings (Hunter & Maunder, 2001). It is asserted that a person’s attachment status becomes more of a behavioural influence in a situation such as a visit to a doctor (Thompson & Ciechanowski, 2003). This is because ill health usually promotes feelings of anxiety and perceived vulnerability which are similar to circumstances when the attachments were originally formed. A medical consultation involves two parties and engaging in discussion of emotional discourse is also challenging for doctors who often employ strategies to avoid discussing psychosocial factors (Maguire & Pitceathly, 2002). According to attachment theory, the relationship model that doctors have may also explain how likely they are to engage in emotional discussion and therefore their interaction with patients. Research shows that there is a relationship between doctor attachment status and their ability to react therapeutically to patients (Dozier et al., 1994). Securely attached doctors had the capacity to reflect on what the patient revealed and were much more responsive to a patient’s underlying needs compared to insecurely attached doctors. Insecurely attached doctors responded to the patient’s more obvious needs but seemed less inclined to investigate more subtle and potentially emotional needs (Dozier et al., 1994).
Similar findings have also been shown amongst mental health carers, with those who were rated as securely attached being more empathetic towards their clients than those with insecure attachment styles (Dozier et al.,1994). This effect has been demonstrated even amongst counsellors who are still training (Trustyet al., 2005). This is an important finding since it at this point that it is most possible to introduce an educational intervention. However, the relationship of attachment style on empathic communication has never been explored amongst medical students. Communication training is now a core part of all medical training so there is enormous scope for educational intervention should an effect be found.
The aim of this study was to test whether securely attached medical students respond to patients’ cues and concerns in a more explicit and inviting manner compared with insecurely attached students. If expectations are confirmed, educational interventions and medical training should be informed (Salmon and Young, 2005).
Method
Participants
A cohort of first year medical undergraduates at a UK medical school was invited to take part in the study during the first week of their undergraduate training. All of the 281 students approached consented to take part. For the purposes of this study, a random sample of 82 participants was selected. This sample consisted of 35 females (42.3%) and 47 males (57.7%) with ages ranging from 17-34 years and a mean age of 20 years.
Design
This study adopted a between-groups analysis to compare the responses of securely attached student doctors to insecurely attached student doctors when presented with patients’ cues and concerns. The independent variable was attachment status (secure or insecure) and the dependant variable was type of response.
Measures
Each student completed The Relationship Questionnaire (Bartholomew & Horowitz, 1991), which includes 30 items from which students are categorised as securely or insecurely attached. The video taped interviews were rated based on the systems defined in Verona: Coding Definition of Emotional Sequences (VR-CODES) (Del Piccoloet al., 2008). This coding scheme was developed at the Verona Network on Sequence Analysis (Del Piccoloet al., 2005), with the objective of developing consensus definitions for patients’ cues/concerns and doctors’ responses to these. The scheme is divided into two areas, firstly to identify and code the cues or concerns of the patient and secondly to code the responses of the providers.
The coding scheme defines a cue as a verbal hint suggesting unpleasant emotion. Examples include metaphorical cues such as ‘My head is throbbing’ and physiological cues such as ‘I can’t sleep’ or ‘I have no appetite.’ A concern is a clear verbalisation of an unpleasant state. Examples include explicit statements such as ‘I’m depressed’ or ‘I can’t cope.’ The second part of the coding manual refers to the provider’s responses to the patient’s cue/concern. There were three levels of responses that are displayed in the diagram below (Figure 1).
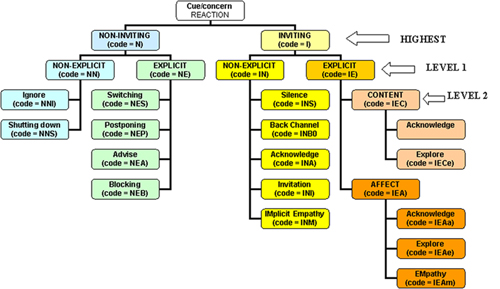
Figure 1. Healthcare provider responses to patients’ cues/concerns. Adapted from Del Piccolo, Finset & Zimmermann (2008).
At the highest level, the doctor was coded as being inviting or non- inviting. At level 1 responses were rated as one of four options: non-inviting non-explicit, non-inviting explicit, inviting non-explicit or inviting explicit. Level 2 is the most detailed coding for individual responses. Table 1 gives a few examples of how responses would be coded using this scheme.
|
Non-Inviting Non Explicit Ignore (NNI) Pt.: I am so worried about the operation that is scheduled for Friday. Dr.: OK, are you still on antibiotics? |
|
Non- Inviting Explicit Switching (NES) Pt: I was really worried about the operation Dr: How does your husband feel about it? |
|
Inviting Non Explicit Back Channel (INB) Doctors Responses such as: Mmm, Yes or Right |
|
Inviting Explicit Affect (IEA) Pt.: I am so worried about the operation that is scheduled for Friday. Dr.: What it is that worries you about the operation? |
Table 1. Examples of coded responses
Inter-rater reliability
In order to gain reliability, the authors (three final year undergraduates) were trained on the scheme. In order to gain inter-rater reliability, undergraduates had a series of training meetings with two senior researchers, Dr Sarah Peters, senior lecturer and the research project supervisor and Dr Ian Fletcher, a member of the Verona Network Team that had originally developed the VR-CODES coding system. During training, each researcher coded a selection of transcripts from video tapes and disagreements were resolved through discussion with reference to the coding manual. Following training, each author independently coded 11 videos. These were then compared to ‘gold-standard’ ratings and inter-rater reliabilities calculated (see Table 2). Gold standard ratings were provided by Dr Ian Fletcher. (Del Piccolo et al., 2008).
|
|
Rater |
||
|
|
KA |
AC |
LR |
|
Patients Cues and Concern †< /strong> Cues Concerns |
.70 .96 |
.92 .88 |
.84 .93 |
|
Doctor responses# Inviting (I) vs Non-Inviting (NI) Explicit (E) vs Non-Explicit (NE) Level 1 (E-I, E-NI, NE-I, NE-NI) Level 2 (13 categories) |
.92 .67 .73 .66 |
.72 .73 .70 * |
.92 .62 .73 * |
Table 2. Inter-rater comparisons with gold-standard ratings
†Intraclass correlations, #Kappa coeffients, *cannot be computed due to uneven tables Using Cohen’s Kappa a score of 0.60-0.80 is considered a substantial agreement between raters and a score of 0.8- 1 is considered almost perfect agreement (Landis & Koch, 1977).
The inter-rater reliability scores were deemed satisfactory (Intraclass correlations from all members were above .70 for cues/concerns and Kappa coefficients above .60 for responses) so the team continued to code the samples. Each undergraduate coded 26 video tapes giving a total of 78 videos. The research team were blind to the attachment status of the student doctor so as not to be influenced when rating.
Procedure
Interviews were a standard experience for a student starting medical training at Liverpool University. Their purpose was to asses the initial communication abilities of each student and to give the student an opportunity to practice interacting with a patient. Each student was instructed to interview one of two simulated patients (SPs) for five minutes, as though they were on an attachment at a GP placement as a first year medical student. SPs are actors trained to be patients and are used commonly in communication training for healthcare providers (Linssen et al., 2007; Shankaret al., 2006). Each SP presented a physical symptom with an underlying psychosocial cause (tension headache or fatigue caused by low mood). Both scenarios were designed to provide students with a similar frequency of empathic opportunities. The two different scenarios allowed for the findings to be generalised across gender and health complaints. Students were randomly assigned to either scenario A or scenario B. Before the video, students completed a brief questionnaire measure to assess attachment status (Bartholomew & Horowitz, 1991). Videos were subsequently coded by the authors who were blind to the attachment status of the students. All interviews were videotaped for subsequent coding and analysis. Using SPs enabled us to control for a number of variables that using a real patient-doctor setting would have disallowed – e.g., length of interview, experience of the student doctors and having the same brief prior to the interview to ensure consistency throughout the interviews.
Ethics
The recordings of the student doctors and SPs had approval from Liverpool University Ethics Committee which involved a student academic representative being involved in the discussion of the design. Informed consent was gained from each of the participants and feedback was given from a communications lecturer after completion of the interviews. All of the student doctors were allocated individual ID numbers to ensure anonymity.
Statistical Analysis
Initial analysis included tests for normality and demographic descriptive statistics. Independent T-tests were conducted to establish whether significant differences existed between the highest level responses (inviting, non-inviting, explicit and non-explicit) for secure and insecure attachment styles.
Results
Results from The Relationship Questionnaire (Bartholomew & Horowitz, 1991) indicated that 48.8% of the sample had a secure attachment status (40 student doctors) and 51.2% had an insecure attachment status (42 student doctors). Tests for normality were conducted on the data and normal distributions confirmed. In total, 323 cues (mean per interaction=3.94, SD=2.03) and 158 concerns (mean per interaction=1.93, SD=0.95) were identified (total=481 cues/concerns, mean per interaction=5.87, SD=2.03). Both SP’s offered similar numbers of cues/concerns within interactions (t=1.21, df=80, p>.01). Table 3 presents the responses to cues/concerns by the student doctors.
|
Response |
N |
% |
Mean |
SD |
|
Non Inviting-Non Explicit |
42 |
8.71 |
.51 |
.93 |
|
Ignore |
38 |
7.88 |
.46 |
.88 |
|
Shutdown |
3 |
.62 |
.04 |
.25 |
|
Non Inviting- Explicit |
161 |
33.4 |
1.96 |
1.58 |
|
Switch |
119 |
24.69 |
1.45 |
1.5 |
|
Postpone |
1 |
.21 |
.01 |
.11 |
|
Advise |
41 |
8.51 |
.50 |
.72 |
|
Block |
9 |
1.87 |
.11 |
.57 |
|
Inviting- Non-Explicit |
64 |
13.28 |
.78 |
1.32 |
|
Backchannel |
41 |
8.51 |
.50 |
1.03 |
|
Invitation |
9 |
1.87 |
.11 |
.42 |
|
Implicit Empathy |
1 |
.21 |
.01 |
.11 |
|
Inviting- Explicit |
214 |
44.4 |
2.6 |
2.17 |
|
Content |
159 |
32.99 |
1.94 |
1.56 |
|
Affect |
60 |
12.45 |
.73 |
1.22 |
Table 3. Responses to cues/concerns
Independent T-tests were conducted to see whether there was a significant difference between mean level 1 responses for secure and insecure attachment styles. There were no significant differences in the type of response made by secure and insecure doctors:
Inviting Responses
There was no significant difference in the number of inviting responses between securely attached student doctors (M=3.13, SD=2.90) and insecurely attached student doctors (M=3.13, SD=3.71) (t=0.192, df=80, p> .05).
Non-Inviting Responses
There was no significant difference in the number of non-inviting responses between securely attached student doctors (M=2.75, SD=2.72) and insecurely attached student doctors (M=2.05, SD=2.26) (t=0.077, df=80, p> .05.).
Explicit Responses
There was no significant difference in the number of explicit responses between securely attached student doctors (M=4.60, SD=3.26) and insecurely attached student doctors (M=4.28, SD=2.81) (t=0.509, df=80, p> .05).
Non-Explicit Responses
There was no significant difference in the number of non-explicit responses between securely attached student doctors (M=1.60, SD=2.81) and insecurely attached student doctors (M=1.26, SD=2.26) (t=.396, df=80, p> .05).
Discussion
Contrary to expectations, our results do not support the hypothesis that attachment style predicts responses to cues/concerns within an analogue clinical interaction. Specifically, the hypotheses that securely attached student doctors use more inviting responses than insecurely attached student doctors was not supported. The present findings are explored by considering potential theoretical and apparent methodological flaws.
This is the first study to address how relationship models affect empathic responses of student doctors. However, research using counselling students supports that positive attachment styles predict empathic responses to emotional issues (Trustyet al., 2005). The present findings do not support such research, or the thesis that securely attached individuals are able to draw upon a bank of positive experiences to which insecurely attached individuals do not have access (Jones, 2005). In previous studies securely attached individuals are shown to have the ability to be assertive and open in interactions; to express and understand empathy; to be more efficient and expressive regarding emotions as well as being more skilled when dealing with difficult emotions. These are all characteristics that researchers expect to not only be more available to securely attached individuals but also to be used more often within interactions (Anders and Tucker, 2000; Fivush, 1991; Guerro, & Jones, 2003; Jones, 2005; and Trusty et al., 2005). The unexpected findings of the current study may therefore relate to particular methodological limitations of the study.
One methodological limitation of the study relates to the participant sample because experimental designs may be considered artificial when student doctors and SPs are used instead of practising doctors and patients (Cohen et al., 2003). Some studies argue that student doctors behave differently with simulated versus real patients and therefore the predictive value of using simulated situations to relate to real medical settings is low (Pieterset al., 1994). However, this point of view has been strongly contested. Evidence suggests that both practising and student doctors cannot distinguish between SPs and real patients (Baerheim and Malterud, 1995;McAvoy, 1988; and Normanet al., 1985). Also, a small body of evidence suggests that SPs are very realistic, so much so that playing the role can result in experiencing symptoms themselves (Bokkenet al., 2004). Furthermore, using SPs allows researchers to control for and manipulate different variables such as sex and age, which strengthens experimental design - an occurrence observed within the present study. Much research therefore suggests that there is little advantage to using real patients rather than SPs (Cohen et al., 2003).
Furthermore, researchers maintain that SPs are widely used because they play a valuable role in assessing clinical communication skills (Linssenet al., 2007; and Shankaret al., 2006). Also, barriers that prevent studying real world clinical interactions have been identified and include reluctance from doctors and patients to participate in experiments and time constraints within the GP practice (Hall, 2003). In addition, certain ethical considerations may prevent real patients from engaging in interactions with untrained student doctors. This is particularly true for students embarking on clinical training, such as the students in our study. Although there is debate as to the validity of SPs and student doctors involved in clinical communication research, the barriers that prevent access to the study of doctor-patient interaction in natural settings make simulated situations the most appropriate method of study at present (Hall, 2003).
Nevertheless, it is still important to consider factors involving SPs and student doctors that might encumber the present study. By examining the video data in depth, it was possible to make observations about the participants’ communicative patterns. Firstly, it was recognised that cues/concerns presented by SPs were often explicit and clear. Although real patients are likely to make obvious hints to emotional issues on occasion, the SPs may have been helping student doctors with the flow of the interaction at times, especially when the student doctor was struggling. In one example, a student doctor breaks down by laughing awkwardly and staring at the camera, an uncomfortable silence follows. In this situation, the SP offers additional cues that are very clear, ‘so… I’ve just moved over from Manchester, about six months ago, left all my family and friends’. The SP emphasised this sentence and reassured the student doctor by smiling. This behaviour might have resulted from the SP feeling uncomfortable or sympathetic towards the medical student, and taking into account that the student was very inexperienced. However, this behaviour would be much less likely to occur in natural doctor-patient interactions and thus supports the evidence that argues that SPs contribute to artificial settings that are not necessarily generalisable (Pieters et al., 1994). Furthermore, the number of cues/concerns and also responses would potentially have differed if the SP had not intervened in this type of instance. Given that frequencies of cues/concerns and responses are central to the present analysis, prompting student doctors with cues or concerns gives participants an unfair advantage, possibly influencing results.
Another important methodological issue to consider involves the coding manual used. Raters did reach adequate levels of inter-rater reliability (all above .60) providing reliability at ‘gold standard’ for the SP’s cues and concerns. However, the coding system used (Del Piccoloet al.’s 2008 VR-CODES) was being developed alongside the current study, hence limiting the training undertaken by the research team. Further improvements to the coding manual have emerged since this study as part of ongoing development. The fact that the coding manual was under development meant that the research team had to re-familiarise themselves with the coding criteria on numerous occasions during training. Future research should replicate the study using a more current revision of the coding system.
A further potential concern was that non-verbal communication (NVC) was not included in analysis. This should be considered for future researchbecause a large body of research suggests that NVC is an important contributory factor when assessing communication (Ishikawaet al., 2006).Specifically, many researchers argue that studying NVC within clinical interactions is vital because it contributes to how responses will be interpreted and should not be left out of any interaction rating systems (Ishikawa, et al., 2006). Hence, future research would be wise to explore to what extent NVC influences doctor responses. However, it is very difficult to code NVC and the use of NVC would have been too time consuming for use within the present study. Furthermore, the current hypothesis relates specifically to dealing with the content of conversation.
Researchers are eager to explore the influence that the characteristics of the doctor, and in particular attachment style, have on aspects of clinical communication (Ciechanowski et al., 2004; Hall, 2003; and Salmon & Young, 2005). Although the present findings are do not prove the hypothesis, they do reflect the complexity of the issue. Nevertheless, research into attachment style and the responses of health providers is in its infancy and requires further attention to methodological difficulties. Similar studies that did not always observe expected results maintain that the attachment theory can be successfully applied to understanding health provider responses (Trusty et al., 2005). Thus, it is crucial to maintain interest in this subject in order to allow our understanding to progress and future practical applications of theory to benefit.
References
Ainsworth M., M. Blehar, E. Waters and S. Wall (1978) ‘Patterns of attachment: apsychological study of the Strange Situation’. Cited in: Ciechanowski P., E. Walker E, W. Katon and J Russo (2002) ‘Attachment Theory: A Model for Health Care Utilization and Somatization’, Psychosomatic Medicine,64, 660-667
Anders, S., and J. Tucker (2000), ‘Adult attachment style, interpersonal communication competence, and social support’, Personal Relationships, 7(4), 379-389
Baerheim, A. and K. Malterud (1995), ‘ Simulated patients for the practical examination of medical students: Intentions, procedures and experiences’, Medical Education, 29 (6), 410–4 13
Bartholomew, K. and L. Horowitz (1991), ‘ Attachment styles among young adults: a test of a four-category model’, Journal of Personality and Social Psychology,61, 226-44
Bartholomew K. (1993), ‘From childhood to Adult Relationships: Attachment Theory and Research’. Cited in: Ciechanowski P., E. Walker, W. Katon and J Russo (2002), ‘ Attachment Theory: A Model for Health Care Utilization and Somatization’, Psychosomatic Medicine,64, 660-667
Bokken, L., J. V. Dalen and J-J. Rethans (2004), ‘Performance-related stress symptoms in simulated patients’, Medical Education, 38(10), 1089-1094
Boseley, S. (2008), NHS: BMA agrees need to check doctors' fitness to practise, http://www.guardian.co.uk/society/2008/jul/24/nhs.health, accessed 24 July 2008
Bowlby, J. (1973). ‘Attachment and loss: Vol. 2. Separation: Anxiety and anger’. New York: Basic Books
Ciechanowski P., E. Walker, W. Katon and J. Russo (2002), ‘Attachment Theory: A Model for Health Care Utilization and Somatization’, Psychosomatic Medicine,64, 660-667
Ciechanowski, P., J. Russo, W. Katon, M. Von Korff, E. Ludman, E. Lin, G. Simon and T. Bush (2004), ‘ Influence of patient attachment style on self-care outcomes in diabetes’, Psychosomatic Medicine, 66 (5), 720-728
Cohen, L., W. F. Baile, E. Henninger, S. K. Agarwal, A. P. Kudelka, R. Lenzi, J. Sterner and Marshall, G. D. (2003),‘ Physiological and psychological effects of delivering medical news using a simulated physician-patient scenario’, Journal of Behavioral Medicine, 26 (5), 459-471
Dacre, J., J. Richardson, L. Nobel, K. Stephens and N. Parker N (2004), ‘Communication skills training in postgraduate medicine: the development of a new course’, Postgraduate Medical Journal,80, 711-715
Del Piccolo, L., Goss, C., and Zimmermann, C. (2005), ‘The third meeting of the Verona Network on Sequence Analysis: Finding common grounds in defining patient cues and concerns and the appropriateness of provider responses’, Patient Education and Counselling,57, 241-244
Del Piccolo, L., Finset, A., and Zimmermann, C. (2008) On behalf of the Verona Network on Sequence Analysis. ‘Verona: Coding Definition of Emotional Sequences (VR-CODES). European Association for Communication in Healthcare
Dozier M., K. Cue and L. Barnett (1994), ‘Clinicians as caregivers: Role of Attachment Organization in Treatment’, Journal of Consulting and Clinical Psychology,62, 793-800
Eagles, J. M., S. A. Calder, K. S. Nicoll and P. D. Sclare (2001), ‘Using simulated patients in education about alcohol misuse’, Academic Medicine, 76 (4), 395
Engel, G. (1977), ‘The Need for A New Medical Model’, Science196 ,129-136
Fivush, R. (1991), ‘Gender and emotion in mother–child conversations about the past’< /span>, Journal of Narrative and Life History, 1(4), 325–3 41
Grifin S., L. Kinmonth, M. Veltman, S. Gillard, J. Grant and M. Stewart (2004), ‘Effect on Health-Related Outcomes of Interventions to Alter the Interaction Between Patients and Practitioners: A Systematic Review of Trials’, Annals of Family Medicine 2, 6
Guerrero, L. K. and S. M. Jones (2003), ‘ Differences in one’s own and one’s partner’s perceptions of social skills as a function of attachment style’, Communication Quarterly, 51 (3), 227-295
Hall, J. (2003), ‘Some observations on provider-patient communication research’, Patient Education and Counseling, 50 (1), 9-12
Halpern J. (2003), ‘What is clinical empathy?’, Journal of General Internal Medicine,18, 670-674
Hunter J. and R. Maunder (2001), ‘Using attachment theory to understand illness behaviour’, General Hospital Psychiatry,23, 177- 182
Ishikawa, H., H. Hashimoto, M. Kinoshita, S. Fujimori, T. Shimizu, and E. Yano (2006), ‘Evaluating medical students’ non-verbal communication during the objective structured clinical examination’, Clinical Competence,40 (12), 1180-1187
Jones, S. M. (2005), ‘Attachment style differences and similarities in evaluations of affective communication skills and person-centred comforting messages’, Western Journal of Communication, 69 (3), 223-249
Landis, J.R. and Koch, G. G. (1977) ‘The measurement of observer agreement for categorical data’, Biometrics. Vol. 33, pp. 159--174
Lang F., M. Floyd and K. Beine (2000), ‘ Clues to patients’ explanations and concerns about their illnesses. A call for active listening’, Archive of Family Medicine, Vol. 9
Linssen, T., J. V. Dalen and J-J. Rethans (2007), ‘Simulating the longitudinal doctor-patient relationship: experiences of simulated patients in successive consultations.’ Medical Education, 41 (9), 873-878
Maguire P. and C. Pitceathly (2002), ‘ Key communication skills and how to acquire them’, British Medical Journal, 325, 697-700
McAvoy, B. (1988), ‘Teaching clinical skills to medical students: The use of simulated patients and videotaping in general practice’< /span>, Medical Education, 22, 193–1 99
Nordin T., A. Hartz, R. Noyes, M. Anderson, M. Rosenbaum, P. James, J. Ely, N. Agarwal and B. Levy (2006), ‘Empirically identified goals for the management of unexplained symptoms’, Family Medicine,38 (7), 476-482
Norman, G. R., V. R. Neufield, A. Walsh, C. A. Woodward and G. A. McConvey (1985), ‘Measuring physician performance by using simulated patients’, Journal of Medical Education, 60, 925–9 34
Ong L., J. De Haes, A. Hoos and F. Lammes (1995), ‘Doctor- Patient Communication: A Review of the Literature’, Social Science and Medicine,40 (7), 903-918
Peters, S., A. Rogers, P. Salmon, L. Gask, M. Towey, R. Clifford, C. Dowrick, R. Morriss (2009), ‘What do patients choose to tell their doctors? Qualitative analysis of potential barriers for managing unexplained symptoms’, Journal of General Internal Medicine, 24 (4), 443-449
Pieters, H., M. Touw-Otten and R. De Melker(1994), ‘ Simulatedpatientsin assessing consultation skills of trainees in general practice vocational training: A validity study’, Medical Education, 28 (3), 226-233
Roter D., S. Stewart, N. Putnam and M. Lipkin (1997), ‘Communication patterns of primary care physicians’, Journal of the American Medical Association, 277, 350-6
Safran D., D. Taira, W. Rogers, M. Kosinski, J. Ware and A. Tarlov (1998), ‘Linking primary care performance to outcomes of care’, Journal of Family Practice,47, 213-219
Salmon, P., and B. Young (2005), ‘Core assumptions and research opportunities in clinical communication’, Patient Education and Counseling,58 (3), 225-234
Shankar, P. R., P. Subish, A. K. Dubey and P. Mishra (2006), ‘Postgraduate students as simulated patients in communication skills learning assessment’, Pharmacy Education, 6 (3), 157-159
Simpson M., R. Buckman, M. Stewart, P. Maguire, M. Lipkin, D. Novack and J. Till (1991), ‘Doctor-patient communication: the Toronto consensus statement’, British Medical Journal, 303 (6814), 1385–1 387
Thompson D. and P. Ciechanowski (2003), ‘ Attaching a New Understanding to the Patient- Physician Relationship in Family Practice’, Journal of the American Board of Family Practice,16, 219-26
Trusty, J., K-M. Ng and R. E. Watts (2005), ‘Model of Adult Attachment on Emotional Empathy of Counselling Students’, Journal of Counseling and Development, 83 (1), 66-77
Wittink, Barg and Gallo (2006), ‘ Unwritten Rules of Talking to Doctors About Depression: Intergrating Qualitative and Quantitative Methods’, Annals of Family Medicine, 4, 4
To cite this paper please use the following details: Atherton, K., Chisholm, A., Rutter, L., Peters, S. and Fletcher, I. (2009), ‘Breaking Barriers in Clinical Communication: Are Securely Attached Doctors More Empathetic Doctors?', Reinvention: a Journal of Undergraduate Research, Volume 2, Issue 1, http://www2.warwick.ac.uk/go/reinventionjournal/issues/volume2issue1/atherton Date accessed [insert date]. If you cite this article or use it in any teaching or other related activities please let us know by e-mailing us at Reinventionjournal at warwick dot ac dot uk.
© Reinvention: a Journal of Undergraduate Research (2009). Full copyright remains with the author.