by Nanna Fukushima
The Great Smog of London in December 1952, which caused the premature death of thousands of citizens, brought debate about the adverse impacts of air pollution to an abrupt end. The clear evidence linking air pollution to death set aside previous concerns about the importance of coal to produce energy and heat, and the immense popularity of open fires, and led to the swift passing of the 1956 Clean Air Act. Until that point, the population density of the UK and its heavy reliance on coal had made parts of the country some of the most polluted places in the world.
Efforts to reduce pollution coincided with a significant fall in post-war infant mortality. Infant mortality in England and Wales declined from over 40 deaths per 1000 live births at the end of the Second World War to around 7 deaths per 1000 live births four decades later. However, the role of enhanced air quality in the improvement of infant health is not yet fully understood. Moreover, most contemporary research on the effect of air pollution on health comes from developed countries, where air pollution is comparatively low. Understanding the health impacts of improved air quality in the highly polluted, heavily populated, industrialised cities of 1950s Britain, where solid fuel was the primary source of air pollution and individual households were large emitters, could present a useful parallel for many developing countries today.
To investigate the causal effect of high-level air pollution on infant health, I study the impact of a zonal banning of house coal (bituminous coal) on infant mortality in urban areas in England after the passing of the 1956 Clean Air Act. The Clean Air Act was enacted at the very height of UK coal dependency and prohibited the emission of dark smoke from industries. More importantly, it gave local authorities the mandate to create so-called Smoke Control Areas (SCAs) that banned any smoke emission of any colour from any premises. An owner or an occupier of a building could replace house coal with a non-smoke emitting fuel alternative – such as anthracite and manufactured smokeless fuel – to comply with the regulation. Households were also entitled to receive a reimbursement covering 35–70% of the cost of any building works necessary to comply with the regulation.
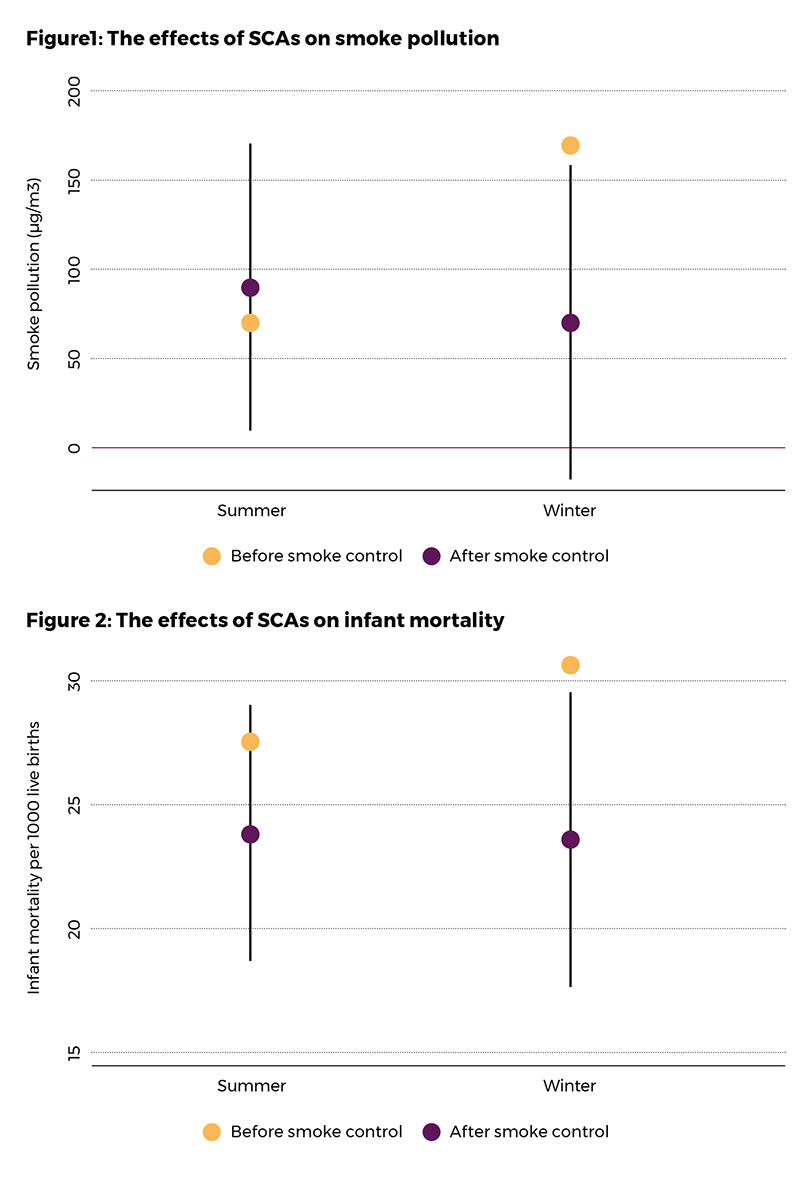
To evaluate the effect of the regulation on local air pollution and infant mortality, I first calculate the effect of a gradual expansion of SCAs between 1957 and 1973 for the winter and summer seasons separately. Since the demand for coal was substantially lower in the summer, we would expect the SCA effect to be negligible during the warm season. Indeed, my analysis reveals that SCAs did not affect summer pollution once we control for place and time characteristics. This method, however, does not account for place-and-time-varying factors affecting pollution and infant health. Therefore, next, I compare the local impact of SCAs in the winter season to the summer season to remove the influence of location specific trends common across the seasons. Figures 1 and 2 show a visual representation of the findings. The pre-regulation levels of smoke-pollution concentration and mortality by season (yellow circles) show how air pollution and infant mortality were much higher in the winter than in the summer. However, after the SCA roll-out, winter pollution and mortality declined, with the post-intervention levels (purple circles) no longer showing any statistical differences across the seasons (95% confidence interval). Given the average SCA coverage, the analysis shows that SCAs accounted for 18% of the decline in smoke pollution and 15% of the decline in infant mortality over the period.
In a further step, I link the effect of improved air quality to infant mortality. To separate the effect of pollution from other unobserved factors that may explain the reduction in pollution and infant mortality, I focus on the impacts of improved air quality brought about as a direct result of SCAs. The method ensures that the estimates are free from the influence of other mortality-reducing effects. I find that smoke particles released from the burning of coal are directly responsible for infant mortality. The effect size implies that for every one microgram per cubic metre reduction in smoke pollution, infant mortality declined by 0.04 deaths per 1000 live births meaning that it can explain as much as 70% of the aggregate reduction in infant mortality in urban areas in England between 1957 and 1973.
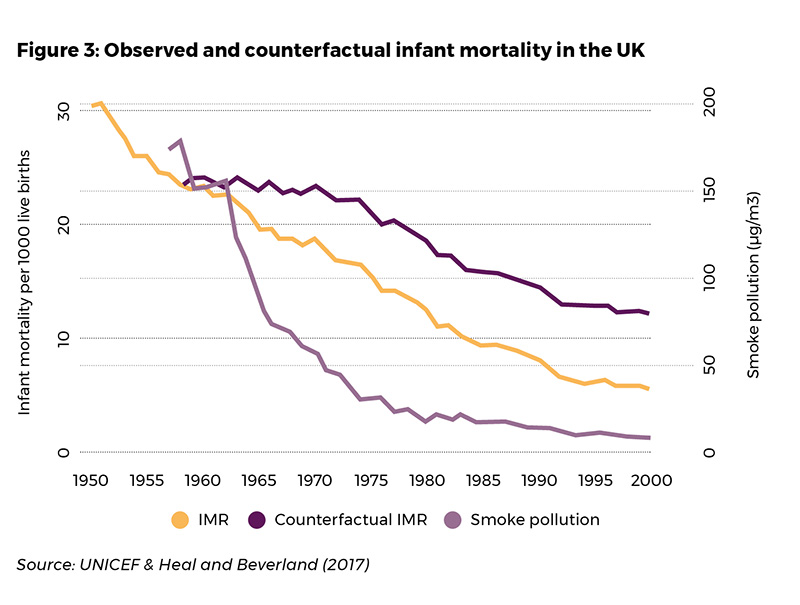
In the study, I also present evidence that the effect of pollution on infant mortality is independent of the initial level of pollution. The findings suggest that we should expect the same change in infant deaths for the same change in air quality irrespective of the location or period of interest. Thus, my results could be used to extrapolate benefits from pollution reduction in developing countries today. To demonstrate the historical role of improved air quality on infant mortality using the study estimates, Figure 3 shows the rate of infant mortality for the whole country had the level of black smoke concentration remained the same as in 1957 (dark purple line).
Other results from the study indicate that the adverse health effects of air pollution are largest for male infants and the youngest infants in particular and that smoke pollution increased the number of miscarriages and stillbirths. Improvement in air quality drove a 10% reduction in prenatal deaths over the sample period and suggests that air pollution's effect on infant mortality is likely a lower bound estimate.
My investigation reveals that improved air quality played a significant role in reducing post-war infant mortality in the UK. The findings are particularly policy-relevant for many high-pollution countries to understand better the impact of air pollution on infant health, which has until now remained unknown.
About the author
Nanna Fukushima is a Post Doctoral Researcher of Economics at the University of Stavanger and a CAGE Associate
Publication details
This article is based on the paper Fukushima, N. (2021). UK Clean Air Act, Black Smoke, and Infant Mortality, CAGE Working paper (no. 587)
