HIV
Health Behaviour in Uganda
Health behaviours, such as taking antiretroviral drugs or using a condom during intercourse, can significantly affect the spread of infection. Although we often know the reduction in an individual's risk of transmitting or receiving an infection if they are taking part in a behaviour, it is more difficult to work out what influences an individual's behaviour and how that behaviour itself spreads through a population.
Our recent work has started to answer these questions using a dataset from Uganda, provided by the Liverpool School of Tropical Medicine. The dataset consists of surveys on health behaviours and demographics carried out across Uganda at multiple timepoints, using a methodology that is cheap enough to be carried out every year and in many Ugandan districts. The high spatial and temporal resolution of the data allows trends in health behaviours to be observed that would be missed in a normal, country-level survey.
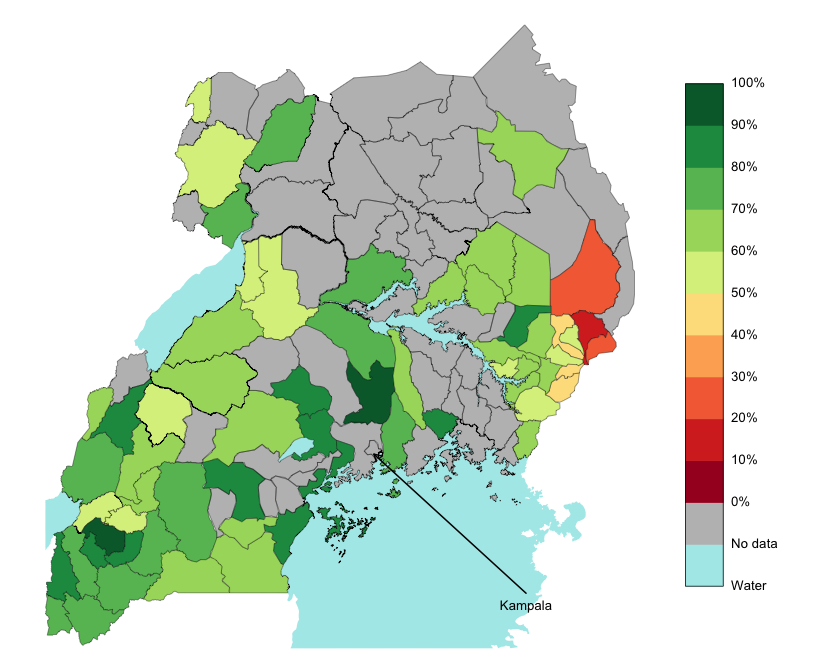 |
| Figure 1. Percentage of mothers who gave birth to their child in a health facility in 2012. Giving birth in a health facility can help prevent the transmission of HIV from mother to child, so understanding and encouraging this health behaviour may well lead to better health outcomes. |
Figure 1 shows the prevalence of one particular health behaviour, mothers giving birth in a health facility, across Uganda in 2012. Since giving birth in a health facility can help prevent the transmission of HIV from mother to child, it is important to understand why the prevalence of this behaviour is less than a quarter in some districts but more than three quarters in others.
Combining data from the survey with geographic information such as number of local health facilities, number of roads and the roughness of terrain in Ugandan districts, and fitting a logistic regression model, we identified various factors which explain the spatial variation of the behaviour prevalence. Mothers who give birth in health facilities tend to be more highly-educated, be younger, and live in districts with more health facilities, more roads and flatter terrain than those who do not. There was also a significant positive time trend, implying that prevalence is improving. The regression model was then used to predict which unsurveyed districts, or districts in the future, are likely to have low prevalence. This provides an 'early-warning' system which can be used to prioritise districts which are more likely to need help.
Our current work involves linking health behaviours directly to health outcomes; in particular, how uptake of health services is influenced by the quality of local health facilities, and therefore what effect improving that quality has on mortality.
Prevalence in high-risk groups in Libya
The dispute resolution in 2003 included an agreement with the European Union on humanitarian cooperation and the development of Libya’s first National HIV Strategy. As part of this members of WIDER helped analyse Libya’s first bio-behavioural survey among men having sex with men (MSM) and female sex workers (FSW).
Respondent-driven sampling was used to estimate the prevalence of HIV, hepatitis B virus (HBV), hepatitis C virus (HCV), and related risk factors among 227 MSM and 69 FSW in Tripoli (FSW recruitment ended prematurely due to the political events in 2011). This necessitated the development of novel mathematical models to infer the underlying prevalence from the sampling methodology.
For MSM we estimated an HIV prevalence of 3.1%, HBV prevalence of 2.9%, and HCV prevalence of 7.3%, and for FSW an HIV prevalence of 15.7%, HBV prevalence of 0%, and HCV prevalence of 5.2%. We detected high levels of risk behaviours, poor HIV-related knowledge, high stigma and lack of prevention programmes. These results must be interpreted in the context of the political situation which prohibited reaching an ideal sample size for FSW.
Epidemiology in developed countries
The prevalence of HIV in different risk groups in developed countries is somewhat paradoxical - in particular, sexual and injecting drug risk appear to interact negatively with each other, which is epidemiologically unusual. We are developing methods motivated by network theory to analyse this effect and optimise targeted interventions.
Publications
Sutton AJ, House T, Hope VD, Ncube F, Wiessing L, Kretzschmar M (2012) Modelling HIV in the injecting drug user population and the male homosexual population in a developed country context. Epidemics 4 48-56
Valadez, J.J., Berendes, S., Jeffery, C., Thomson, J., Ben Othman, H., Danon, L., Turki, A.A., Saffialden, R., Mirzoyan, L. (2013) Filling the Knowledge Gap: Measuring HIV Prevalence and Risk Factors among Men Who Have Sex with Men and Female Sex Workers in Tripoli, Libya. PLoS ONE 8 e66701
Funded by: EPSRC
WIDER people involved
Thomas House
Deirdre Hollingsworth
Dan Sprague
Jo Moir-Thompson
External collaborators
Jo Valadez (Liverpool)
