How the 1918 influenza pandemic exacerbated racial inequalities in South Africa

How the 1918 influenza pandemic exacerbated racial inequalities in South Africa
Friday 8 Jan 2021The 1918 influenza pandemic in South Africa was one of the country’s worst human tragedies. The virus killed an estimated 300,000 South Africans – 6% of the population – within three months. But there were large differences in mortality rates across subgroups, with particularly high numbers of deaths among black South Africans. Johan Fourie and Jonathan Jayes show that poor access to healthcare could explain why.
A train left Cape Town on 28 September 1918 carrying soldiers returning from the trenches of war-fatigued Europe. Soldiers disembarked at all the stops, happy to see family and friends. They could not have foreseen the devastation that lay ahead: Black October, a month in which thousands of South Africans would perish.
The Spanish flu – as it has unfairly become known – devastated the Cape Province. A milder strain, entering South Africa through the port at Durban and reaching the gold mines of the Transvaal, caused almost zero fatalities. But a more virulent version arrived with the disembarking soldiers in Cape Town and spread rapidly.
The virus did not affect everyone equally, however. The mortality rates for black South Africans were higher. Some districts were badly affected, with mortality rates above 100 for every 1000 people; others managed to escape such hardship. We identify the factors that help to explain this large variation in mortality rates (Fourie and Jayes, 2021).
Our hypothesis is that unequal access to healthcare is part of the explanation. South Africa, then as now, was a highly unequal country. This inequality also manifested in access to healthcare. To show this, we transcribe almost 40,000 death certificates from 1915 to 1920. The death certificates record the deceased individual’s biographical information – name, gender, age, occupation, race and address – as well as information on the reason for death and the duration of illness. Each certificate required a doctor’s signature, but often this signature is missing. We use the presence of this signature as evidence of healthcare, the assumption being that if a doctor did not sign the certificate, the individual had no or at least poor access to healthcare.
The transcribed death certificates allow us to, first, ascertain how unequal healthcare provision was both before the pandemic (Jan 1915–Sep 1918) and after it (Feb 1919–Dec 1920). As is clear from Figure 1, there were large differences by race, age and gender. We then investigate whether these differences were exacerbated during the pandemic (Oct 1918–Jan 1919). Figure 1 shows access to healthcare fell sharply across almost all subgroups. Note, in particular, the sharp drop for black South Africans. Using regression analysis, we show that residents described in the death certificate as black and coloured were worse affected than those described as white.
But not all inequalities were exacerbated. In fact, large inequalities that existed for people of a certain age and for certain occupations were reversed. Whereas rural residents had poorer access to healthcare before and after the pandemic, urban residents had poorer access to healthcare during the pandemic. Gender differences were unaffected by the pandemic.
Why is it that race differences were amplified while other inequalities were not? So far we have not found a conclusive explanation. One possibility is that black residents were more likely to live in larger family units – and that the virus spread more quickly within these families. However, when we include a measure of whether a member of the family died in the previous week, the size of the race variable falls but remains significant, suggesting that illness in the family matters but cannot explain the full effect. Proxies for immigrant status, class and location also do not explain away the large race coefficient.
A second option is that perhaps doctors were less willing to treat certain patients during pandemic periods. We use the duration of illness measure to identify racial discrimination: when the duration is bunched around certain dates (one week or one month), it is viewed as a doctor giving less care to a patient. We find no evidence of racial discrimination during the pandemic, confirming anecdotal evidence that race relations were not adversely affected by the Spanish flu.
These surprising results challenge the expectation that all forms of inequality are exacerbated during a health crisis. The case of South Africa shows that while access to healthcare for black South Africans worsened during the Spanish flu pandemic, other inequalities, along the gender, age and occupation dimensions, were not exacerbated and in some cases were even reversed. This evidence may form important lessons for anticipating the effects of the COVID-19 pandemic on equality.
Figure 1: Access to healthcare before and during the pandemic.
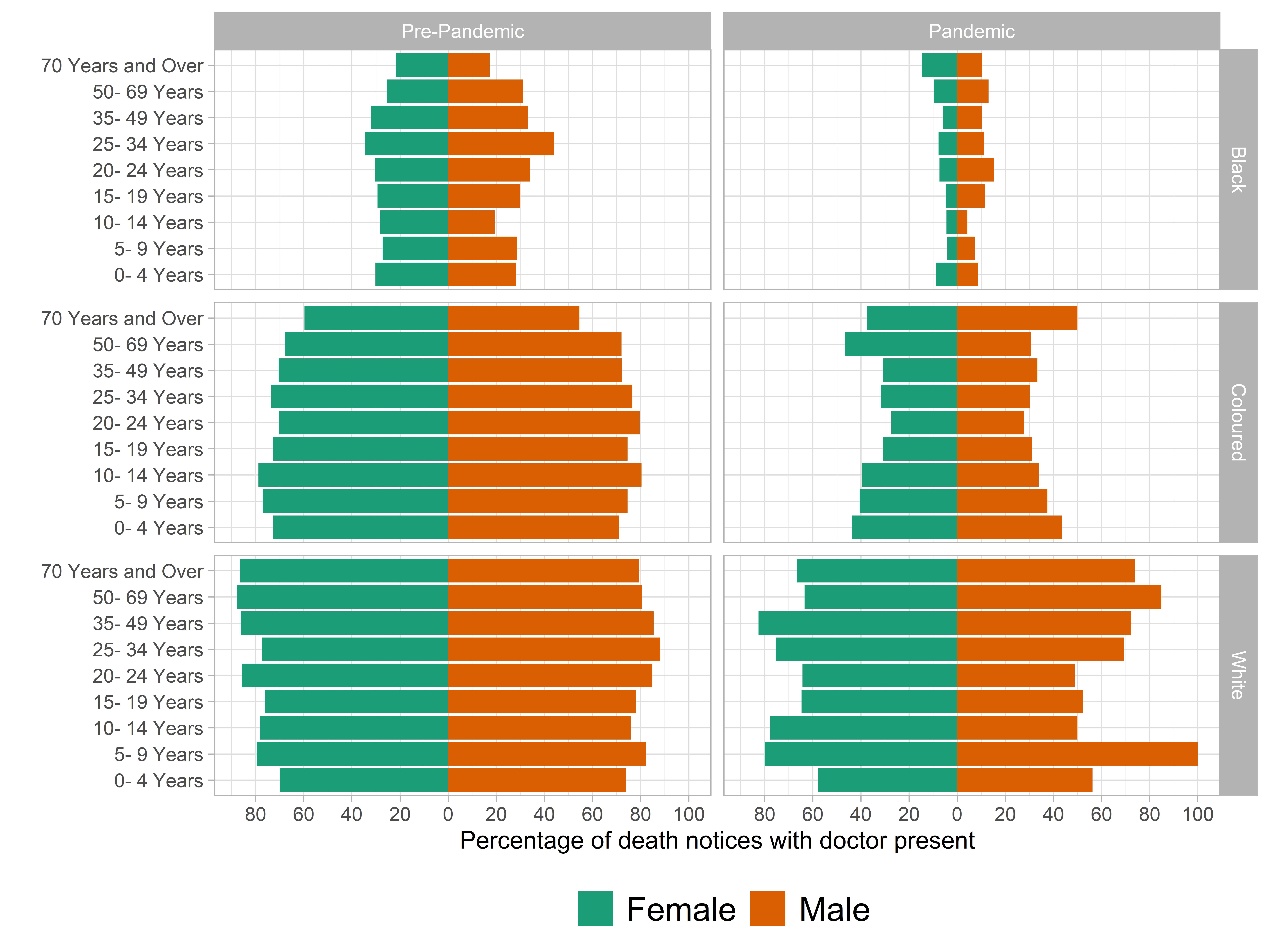
Note: Figure shows the percentage of death certificates signed by a doctor divided by age, gender and race (individuals described on their death certificate as black, coloured or white), for the periods before the pandemic (Jan 1915–Sep 1918) and during the pandemic (Oct 1918–Jan 1919).
Johan Fourie, Stellenbosch University, South Africa
Jonathan Jayes, Stellenbosch University, South Africa
References
Johan Fourie and Jonathan Jayes (2021), Health inequality and the 1918 influenza in South Africa, CAGE Working paper (no.532)
