Short Project Descriptions
Implementation of Remote Consultations – Reducing Inequality of Access
Leads: Dr Kelly-Ann Schmidtke, Dr Laura Kudrna (Meths), Prof Kate Jolly (Public Health), Dr Sarah Damery (Long-term Conditions)
The team are working with four public contributors with experience of remote consultations throughout the project.
Dates: April 2021 - March 2022
Background:
“The NHS Long-Term Plan” (2019) is a five-year plan describing how NHS services should be redesigned for the next decade. This plan includes making better use of digital technologies, such as video consultations. While video consultations have potential advantages for patients and hospital systems, they may make patients uncomfortable. If patients do not walk through the 'digital door' to attend a video consultation, the potential advantages cannot be realised. Likely the motto of “build it and they will come” is insufficient. Instead, we need to support patients so that they come the first time and return after that.
Policy and Practice Partners:
Research around video consultations has been requested by University Hospitals Birmingham NHS Foundation Trust.
Co-Funding Partners:
University Hospitals Birmingham NHS Foundation Trust.
Aims and Objectives:
Defaults have been used to influence people’s behaviour in many contexts, e.g. how much money people save for retirement, physicians’ medication use, and purchases of healthy foods. Re-framing an invitation to attend an outpatient appointment from ‘in-person’ to ‘video’ creates a new default endorsed mode of attendance that is easier to accept. However, if a substantial number of patients refuse an invitation to attend a video consultation, this would suggest that more support is needed to garner people’s acceptance.
Methods:
A total of 1,481 people with a chronic condition living in the UK participated. 53% were female, and their average age was 45 years. 85% had attended a hospital outpatient appointment in the last 12 months, and 27% attended at least one of those appointments via video.
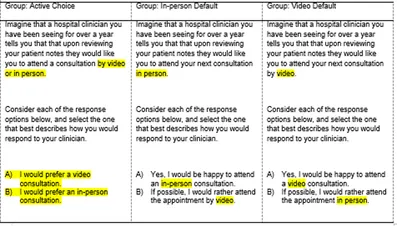
In the survey, participants were randomly assigned to consider one of three hypothetical invitations. Each invitation is provided below with the differences between them highlighted for illustrative purposes.
Main Results (draft):
The graph below displays the proportion of participants in each group who agreed to attend a video appointment.
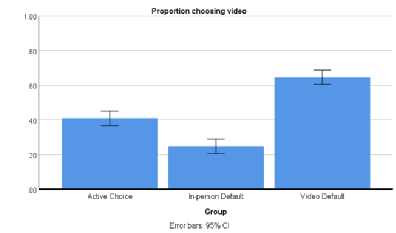
When participants were asked to actively choose an appointment mode, 40% chose video. When an in-person appointment was proposed, only 25% did. When a video appointment was proposed, 65% did. All these percentages are different from each other and from 50%. In a future analysis, we will include participant demographics, including their age, sex, previous experience with video consulting, and diagnostic complexity. A preliminary look suggests that none of these demographics significantly influenced participants’ choices.
Future analyse will also examine how ethnic group and resident UK country influence the results.
Anticipated Conclusions:
The big conclusion will be that the default proposed mode influences participants’ acceptance of video consulting. Tactics will be proposed to build on the perceived advantages and to overcome the perceived disadvantages participants note with regard to video consulting to ensure that the attend their first video appointment and return for future video appointments.
Implications for Implementation:
Where appropriate, hospitals should invite people to attend outpatient appointments via video and this will naturally increase the number of people who attend video appointments. These findings will inform Trusts in how to word invitations to a consultation to support the move towards virtual consultations, in line with the NHS Long Term Plan.