WITHIN Blog: December 2020
#ItTakesGuts – Experiences of Living with Ulcerative Colitis
Written by Paige Karadag, Research Assistant, WITHIN Study
This blog details our own Research Assistant’s experiences of having Ulcerative Colitis. As these are her personal experiences, we understand that they might not reflect your own.
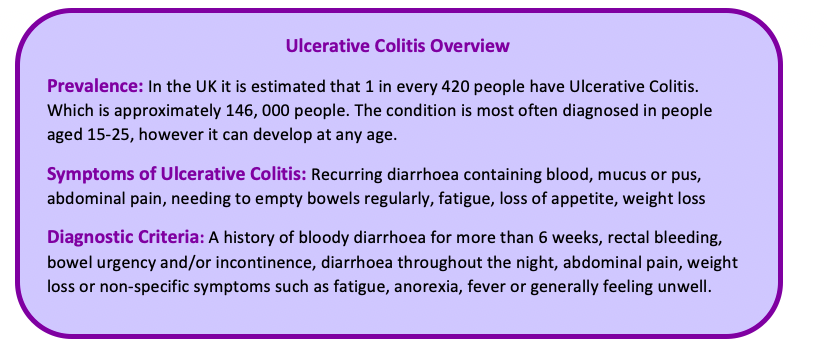
This week, in the UK, it is Crohn's and Colitis awareness week and as part of the #ItTakesGuts campaign, I wanted to share my story with you all. Having Ulcerative Colitis (UC) hasn’t always been easy for me to talk about, but I wanted to share some of my experiences to raise awareness of UC, so that people who have it know that they are not alone. I have lived with UC for six years now, being diagnosed when I was 17 years old, and I will have it for the rest of my life. During this time, I have had a blood transfusion, iron transfusions, tried over ten different types of medications, including tablets, injections, infusions and enemas, had several colonoscopies and narrowly avoided surgery. For those of you that don’t know, UC is a form of Inflammatory Bowel Disease (IBD) and is an autoimmune disease that causes inflammation and ulceration of the colon and rectum. Before I was diagnosed, I had never heard of the terms Ulcerative Colitis or Inflammatory Bowel Disease and at the time I did not really understand the severity of the condition.
During the first year following the diagnosis, my symptoms were almost constant, going to the toilet over fifteen times a day and passing blood each time. As I was applying to universities and studying for my A Levels, I felt that I could not afford to have any time off, so every day I went to sixth-form experiencing these debilitating symptoms and excruciating pain. I told very few of my friends about my diagnosis as I was so embarrassed of the symptoms. I felt very isolated and desperately wanted to be a ‘normal’ teenager, yet I was battling this ‘invisible illness’. I was also tremendously tired as I experienced insomnia as a side effect of the steroids I was prescribed. I have a vivid memory of giving a talk one evening at the sixth-form and I remember feeling so faint and weak that I could barely stand up. That night, I was admitted to hospital with a flare-up, an infection and anaemia. I was so stressed by this flare-up and the impact on my work that I actually continued to do assignments whilst I was in hospital!
I had another flare up just months later, and this time, doctors told me that they would have to start preparing for surgery if my symptoms did not quickly improve. It seemed that I was ‘steroid dependent’ as every time I came off steroids I would have a flare-up. For the next year or so, I tried various types of medications that would either stop working or I would experience severe side effects including signs of liver damage. Eventually, I was put on a combination of an infusion and three types of tablets, that successfully improved the disease activity and I am now in remission. However, despite being in remission I still experience daily symptoms of UC and in many ways I have had to adjust to this ‘new normal’ of living with IBD.

IMAGE VIA PIXABAY
When I moved away for university, I decided to tell my flatmates about my UC. To my surprise, everyone I told was really understanding and I no longer felt embarrassed to talk about it. This was a huge turning point for me and I began being much more open about my condition and in turn I became more accepting of myself. I actually met someone else on my course who had Crohn's disease, and they have remained a close friend since. I now have a much more positive outlook of having UC and not only has it taught me how resilient I can be, it has made me more appreciative of life, good health and the NHS.
This year, lockdown presented new challenges that I had not previously experienced. As I fall in the ‘high risk’ category due to taking immunosuppressant medication, I had to self-isolate for 12 weeks, unable to go outside, except to go to the hospital for infusions and blood tests. This was particularly difficult as I was doing a master’s degree at the time and lived in a one bedroom flat with no garden. As stress can be a clear trigger for worsening my symptoms, I had relied on exercising and going to the gym for years as a way to help reduce stress. This was something that I was now unable to do. Luckily, ‘home workouts’ kept me sane during this time and they are something that I have continued to do since. Even when I was allowed to go outside for walks, I particularly struggled with public toilets being closed, as they are something that I depend on whenever I go out. My journey with ulcerative colitis so far has definitely been a roller coaster ride and I am sure that in the future I will face further challenges, as I never know when the next flare-up might be. Nevertheless, I am forever grateful for the support and understanding shown by my family, friends, work colleagues and IBD medical team.
Written by Paige Karadag, Research Assistant on the WITHIN Study as part of #ItTakesGuts campaign.
Crohn's and Colitis awareness week runs from 1-7 December and is organised by the charity Crohn’s & Colitis UK. The ‘It Takes Guts’ campaign is also part of Crohn’s and Colitis awareness week, which involves people sharing their stories with the hashtag ‘#ItTakesGuts’ to spread awareness and break down the stigma of Crohn’s and Colitis.
If you would require any further support or information regarding Crohn’s Disease or Ulcerative Colitis please see the resources below.
https://www.crohnsandcolitis.org.uk/support
Helpline Service Crohn’s & Colitis UK: Telephone 0300 222 5700 or email helpline@crohnsandcolitis.org.uk
If you have a chronic pain condition such as IBD and are interested in taking part in research, you may find the following useful. We are currently recruiting participants for an online survey (open to chronic pain patients) to investigate how mental defeat contributes to the persistence of chronic pain and its associated distress and disability. If you would like to get involved or if you have any further questions you can email us at: withinstudy@warwick.ac.uk
