A profile of... Dr Hannah James

Dr Hannah James is a Specialist Registrar in Trauma and Orthopaedic Surgery at University Hospitals Coventry and Warwickshire (UHCW) and an NIHR Academic Clinical Lecturer at Warwick Clinical Trials Unit. In 2023 she became the first female Trauma & Orthopaedic surgeon to be awarded the prestigious Hunterian professorship, and she gave her Hunterian lecture at the recent British Orthopaedic Association annual congress. We caught up with her to find out more about her work and her advice for other women thinking about pursuing this specialty.
Tell us a bit about your career journey so far
I qualified as a doctor from Bristol Medical School in 2008 and completed the Academic Foundation Programme in the south west region, before being appointed to the NIHR Academic Clinical Fellowship in Trauma & Orthopaedic (T&O) Surgery on the Warwick rotation in 2010. I completed a Masters degree in Medical Education whilst undertaking the first three years of specialist training, before pausing clinical work to undertake my PhD at WMS. This was funded principally by an Educational Research Fellowship Award from Versus Arthritis, with additional support from the Royal College of Surgeons and the Chancellor’s Scholarship programme.
My PhD work assessed the impact of a simulation training intervention for junior orthopaedic trauma surgeons, using patient-level outcomes. This was a first-in-field study and generated new insights into how surgeons learn complex skills, how these can be improved, and discovered that it is possible to measure the impact of training interventions for surgeons using patient outcomes. This work has led to a variety of publications and awards and it has generated several exciting collaborations and further ongoing projects.
I have had three temporary career breaks along the way for maternity, finished my PhD less than full-time when my children were very young, and I returned to clinical training full-time in 2020. I am now in the final stages of higher specialist training in T&O before becoming a consultant, with a sub-specialist interest in orthoplastic hand surgery. I am working clinically at UHCW and as an NIHR Academic Clinical Lecturer (ACL) at Warwick Clinical Trials Unit.
 What is your focus in your current role? What do you most enjoy about it?
What is your focus in your current role? What do you most enjoy about it?
My current working week is split between clinical work as a surgeon at the hospital and academic work as a lecturer at the university. The focus of my research is on developing and testing surgical education interventions using clinical trials methodology, including modelling complex learning curves. I am also currently working with both UK-based and international collaborators on a variety of other projects in the surgical education research space.
I like the fact that the hospital and university are two very different environments, each with their respective strengths and challenges. I like the variety of the clinical-academic life and find that the enjoyment of each half of the role is enhanced by the other.
For example, in a typical week I will spend a day (or two) in the operating theatre performing surgery, a day in the outpatients clinic seeing new or follow-up patients, a day (or two) at the university meeting with academic colleagues both internal and external to Warwick working on various projects, plus conferences, seminars, training courses etc. So overall it makes for a busy, varied and satisfying working life!
What has been your experience of working in Orthopaedics given that this is traditionally a male-dominated specialty? Do you have any thoughts on how more women could be encouraged into this career path and do you have any tips for those considering it?
I love orthopaedic surgery and mentor several female medical students and resident doctors who are considering it as a career, but there are certainly some challenges which typically impact women differentially.
It is worth understanding that surgical training is long and it takes a further 10-15 years to become a consultant after finishing medical school. We know from national data that women surgeons-in-training are more likely to get negative outcomes in their annual assessments and pass the final speciality exams (to become a consultant) at a lower rate, and are more likely to leave surgical training schemes. Some of this is probably to do with the fact that surgical training generally coincides with the childbearing years, which differentially impacts women. Our societal childcare provision is not easily affordable nor typically flexible enough to support surgical careers, with its long, fixed and irregular working hours.
Stereotypes can also still persist and there is a hidden energy cost to repeatedly having to justify your credentials that yes, you really are the surgeon that will be doing the operation, and not whichever male staff member happens to be in the room at the time.
There are some practical issues with equipment facing the female orthopaedic surgeon, such as surgical instruments handles being too large as they are designed to suit the average male hand-span, and lead x-ray protection gowns being too heavy and not the right shape to properly protect women - there is a well-documented increased breast cancer risk in female surgeons
However, there has been widespread recognition of these issues across the profession and a huge effort is underway from the Royal College of Surgeons and the British Orthopaedic Association, amongst others, to address them. There are more and more women at all levels coming through the ranks and things are certainly changing for the better.
So - what I say to women considering a career in orthopaedics is that yes you absolutely can do it if you want to, but go into it with your eyes open to the challenges, and if you want to have children whilst in training you can do that too but you need the right support around you: partner, childcare, nanny, extended family etc.
I am very fortunate in having an incredibly supportive husband who has borne much of the mental load of raising a family while I have been busy doing surgical exams and long hospital shifts etc, whilst also working full-time himself. He is the only dad in the class parent WhatsApp groups and the school know to ring him first if there is a problem with one of our children as I am probably scrubbed in surgery! We also employ a nanny to help with wraparound childcare as we don’t have local extended family to rely on, and this has been very helpful especially during the school holidays, or those weeks when my husband is travelling away with work and I am doing nightshifts or on call.
They say it takes a village to raise a child, and this is true. Having a family as a female surgeon is very much a team sport!
What does receiving the Hunterian Professorship mean to you?
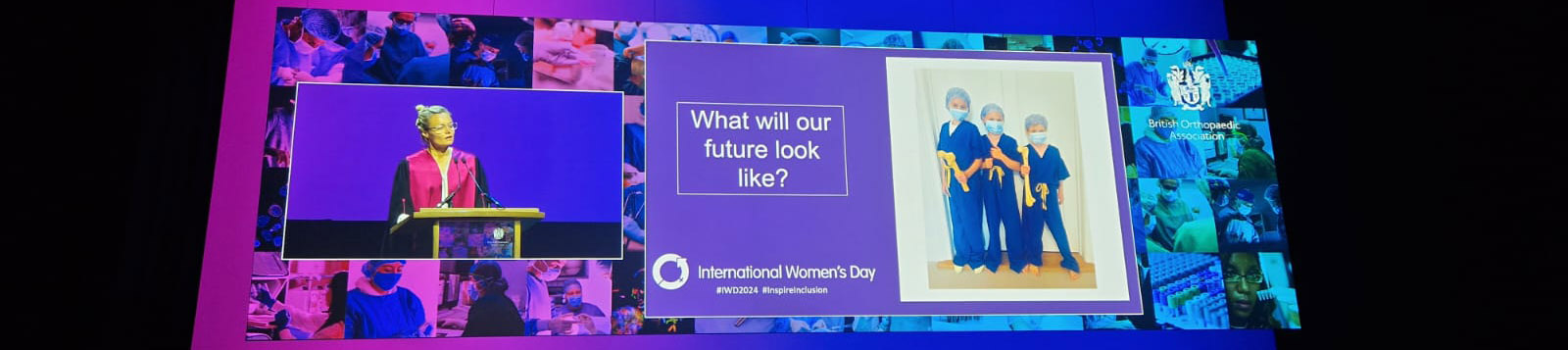
I am very honoured, especially so to be the first female orthopaedic surgeon to become one. There are some big names in surgery, both recent and historic, who have been Hunterian Professors, so to be joining their ranks feels like a huge privilege. I gave my Hunterian lecture at the recent British Orthopaedic Association annual congress, and it was a great platform to be able to showcase my work.
I am aware that I am a visible role model for women in academic orthopaedic surgery and I take that responsibility seriously. I am a firm believer in ‘lift as you climb’ and try to make sure that I bring others with me on the way and help support them navigate the various challenges, as others have done for me. I have been very fortunate to have benefitted from excellent career mentors from diverse backgrounds and I aspire to do the same for others.
What are your ambitions for the future?
I would like to continue working as a clinical-academic orthopaedic surgeon, ultimately at a senior level as a professor, leading a research team delivering trials in surgical education. My ambition is to be doing research that will influence educational policy decision-making at government level and ultimately improve patient outcomes.