Teaching innovation archive
History of MB ChB teaching innovation at WMS
vCBL
Case Based Learning (CBL) is at the core of the whole MBChB curriculum in Warwick Medical School. Small groups of about 8 or 9 students work together discussing a specially written case, taking it in turns to act as chair of the session and to ‘scribe’ mind maps or notes that are shared with the group. The cases combine authentic clinical scenarios with other resources such as clinical imaging, blood tests, clinical guidelines and links to suggested reading, relevant workshops and lectures supporting the topics covered in the case. The students use their prior knowledge and experience to discuss the learning areas in depth and compile a list of topics that they wish to learn more about, appointing a few students to learn about these topics and present on them in the follow up session. Every group also has a facilitator who has been trained to work with small group CBL and have a guide for the case with anticipated learning areas to cover and suggested prompts. Facilitators do not teach the group but, if needed, will prompt further discussion especially if students have not covered an important topic .
Due to the current global Covid-19 pandemic the curriculum needed to be moved online to provide continuity of the course. Virtual online CBL (vCBL) was rapidly developed across all the phases to enable the timetabled CBL sessions to continue as normal. CBL is an ideal real-time (synchronous) activity for learning. The sessions are run via videoconferencing meetings within Microsoft Teams. Trial sessions with a few groups of student volunteers and facilitators confirmed that virtual CBL worked very well and was the perfect opportunity to continue the regular CBL sessions for students despite lockdown. The sessions are similar to the normal CBL except students and facilitators join the meeting from their own location; whether that is on campus or in university accommodation, many are in their homes in the UK and abroad and some have even joined in whilst at work. There are some difficulties with online meetings from WiFi speed to availability of a space to call from. However, there have been many advantages which will benefit the future of CBL at Warwick.
Find out more about our Virtual CBL sessions here.
The students are getting regular contact with their group and a member of staff, the virtual spaces are infinitely larger than a physical building so there is the ability of students to continue working or meeting with each other whenever they wish without the need to book rooms. During the session the students can share their screen to view the case and using PowerPoint slides works really well in this environment. Students can maintain several forms of communication during the session by using the ‘chat’ running down the side of the screen to make additional notes or comment on the case without interrupting the flow of those speaking. Presentations of topics investigated are summarised by students who have used quizzes such as Kahoot or a slide show presentation. The online environment encourages only one person to speak at a time which has focused the discussions and many facilitators find this method is more efficient. Most importantly this will develop the skills of our future workforce who will need the ability to adapt to new technology and to use digital technology and methods of communication in patient care such as video consultations or international MDT meetings via video link.
Mindfulness
Mindfulness is attracting increasing attention as an evidence-based tool that can enhance students’ learning, resilience, compassion and empathy. Research with patient groups has demonstrated that, in conjunction with other healthy living advice, mindfulness can improve outcomes and reduce mortality in serious illnesses.
For these reasons, a universal mindfulness programme was introduced to Warwick medical students in 2013; the first of its kind in the UK. In developing our programme we have had ongoing collaboration with Monash University, Melbourne, where mindfulness programmes have been running successfully for over 20 years. Our own research into the programme has demonstrated that those students who take up regular mindfulness are protected from drops in their wellbeing, even in the face of the stresses of medical training.
Since 2013, mindfulness activities at Warwick Medical School have included…
- Warwick Students’ Mindfulness Society: A student-led group organising world-renowned speakers, retreats, and stress reduction events
- Mindfulness in Health and Higher Education International Conference, 2017: This 2 day international conference, co-produced with Leicester and Buckingham medical schools, brought world leaders in mindfulness research to Warwick.
- Distinguished Visiting Academic programme 2017: Dr. Craig Hassed of Monash University visited this year to help with our faculty development and share good practice
- Staff wellbeing day 2017: Mindfulness was one of the most popular activities at the Warwick Medical School wellbeing day, and there are now plans to put on regular voluntary mindfulness sessions at the medical school for both students and staff.
Medical Education Peer Teaching Programme
In 2019, medical student intern Clarissa Brierley worked with staff to develop a three stage teaching certificate for peer teachers. Warwick has a very strong history of high quality peer teaching with large numbers of students involved and an enthusiasm for teaching. The purpose of developing the certificate was to give students the opportunity to develop their teaching skills through workshops, reflection and peer teaching observation and received recognition for their contribution to life at WMS. The first two runs of level 1 have been oversubscribed and highly rated by students.
We are delighted that Clarissa has been awarded the JASME student innovation prize 2020 in recognition of her work.
Working with patients

In May 2017 we held a workshop based on “Design Thinking” where groups of staff, patients and students joined together to work on solutions to increase the contribution of patients within the curriculum. Four ideas were generated, which we are now working on taking forward:
Patient-based learning
New CBL cases are to be written in conjunction with a patient with the main condition. The case need not be based entirely on the patient’s personal medical problems as this could affect the coverage of required learning objectives, however adding real-life details, more background and more about patient expectation should increase the realism of the case. The patient will record a video clip explaining what it is like to live with the condition.
Role-playing real patients
Patients create scenarios for role playing based on their own experiences of health services. One student role plays the patient, another the doctor. At the end of the scenario they feedback to each other, including their feelings. Session would be recorded for students to watch back afterwards. Again, the patient whose story it is could record a short video for the students to watch afterwards.
The patient journey
Students to accompany a patient to a hospital appointment- starting at the patient’s home. The student would travel on the bus with the patient, sit in the waiting room, observe the appointment and travel back home with them.
Students as feedback facilitators
Students want more direct feedback on how to improve from patients - but patients may feel uncomfortable to give this. Students are on the wards in pairs and would be trained to facilitate feedback. They would ask the patient to give some honest feedback and then give this to their clinical partner.
Student Seminars
WMS has established and high-quality peer teaching organised by students for students which includes basic science sessions, OSCEs and bedside teaching. In 2015 Clare Keith started “Student Seminars” PowerPoint-free teaching sessions, encouraging student teachers to use alternative and more interactive teaching methods such as white boards and educational games. This was presented as a workshop to the University Teaching & Learning showcase and at the WMS conference in 2017. In 2017 Clare was awarded the JASME student innovation award.
Simulation in Medical Education
Simulation in Medical Education, provides a safe place to practise, observe and rehearse communication skills and is an area that is evolving.
Here at Warwick simulation engagement for consultation practise has been utilised from the first days of the Medical School and is expanding to other active learning sessions within the curriculum. Most recently in 2019/20 see the introduction of a student selected component (SSC) study option, Simulation in Medical Education and simulation for intensive care unit training.
The SSC study module involved students working with patients to hear their stories and what was important to them, then using this information to develop OSCE stations where they played the role of simulated patient.
As the demand increases for trained simulators the Warwick Simulation Team has expanded to 70 professional simulators.
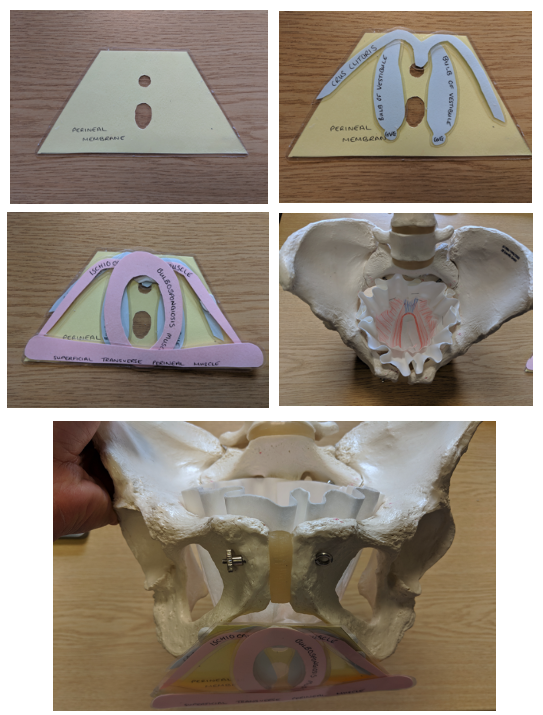
Learning Clinical Anatomy: Through the Act of Drawing & Doing
We are delighted that Dr Erin Fillmore has received the ASME Innovation in Medical Education Award for her work on "Draw it: do it" anatomy teaching. Read more here.Link opens in a new window

Clinical anatomy at Warwick Medical School is taught in a truly innovative way. Our curriculum is designed to ensure students learn, use and apply anatomy in a clinical context. In Year 1 (Phase 1), our multifaceted approach to teaching and learning exposes students to: small group seminars; a unique medical imaging platform; facilitated fresh tissue and plastinated specimen sessions; lecture-theatre based teaching; CBL; clinical skills; and the latest addition to our teaching product, hands-on workshops that require students to interact with clinical anatomy through a set of original activities entitled ‘Clinical Anatomy: Draw-It & Do-It’.
In 2018 the first series of ‘Clinical Anatomy: Draw-It & Do-It’ activities were introduced to Warwick medical students. All such activities are based on topics and concepts that students traditionally find challenging when learning anatomy. The ‘Draw-It’ activities are designed using a framework that guides students to create their own drawings of anatomical structures and/or relationships. The ‘Do-It’ activities include the hands-on manipulation of a conceptual model or a custom-built object that represents core anatomical regions or anatomical processes.
The implementation of the new ‘Clinical Anatomy: Draw-It & Do-It’ sessions into the curriculum is evidence-based. Research shows that both drawing and doing hands-on tasks can help students make sense of complex concepts and explore difficult content. It also helps stimulate meaningful comprehension, and requires students construct their own knowledge based on prior experience. We as educators recognise that clinical anatomy is a challenging subject to learn, but drawing and doing offer yet another way to make the unseen visible and the complex simpler.
Fun Lecture Breaks
Lectures are a common feature of the curriculum in the MBChB course. We trialled the use of interactive lecture breaks to enhance the student learning experience. These breaks involved an optional activity in the form of a Kahoot! quiz on a topic unrelated to the lecture content. Kahoot! is a free and easy-to-use platform and the game-play aesthetic offered by the animations, music and competitive element of a leader board makes it a fun activity for students. Feedback was collected from the students on their perceptions of the activity. Overall student feedback was positive, and they felt that the breaks improved their concentration in the lectures. We will continue to trial different formats of breaks in the upcoming academic year to further improve students’ experience of lectures.

