WMG News
Coronavirus brings dawn of digital healthcare
In light of the highly-infectious Coronavirus pandemic, healthcare systems across the world have had to adapt rapidly for the evolving situation for three reasons:
1. The need to triage and treat large number of patients with respiratory problems
2. The need to protect healthcare workers to ensure they can treat the sick
3. The need to protect the elderly and most vulnerable in society from being infected
In the editorial, 'Covid-19: A new digital dawn?', published in the journal Digital Health (SAGE Publications), researchers from our Institute of Digital Healthcare at WMG, University of Warwick (together with colleagues from Warwick Medical School, University Hospitals Coventry & Warwickshire NHS Trust and Bristol Heart Institute, United Hospitals Bristol NHS Foundation Trust) provide insight into how these three reasons have led to an increase in digital healthcare.
 Professor Theodoros Arvanitis, from the Institute of Digital Healthcare at WMG, University of Warwick comments:
Professor Theodoros Arvanitis, from the Institute of Digital Healthcare at WMG, University of Warwick comments:
“Covid-19 will unfortunately have a human cost that will be remembered for many years to come. Its impact on healthcare, the economy and society, as a whole, will be rather significant. However, it could also be the start of more digitised healthcare, as new ways of remote and digital health working have had to evolve so rapidly. We can learn from this time and take it further to make one positive come out of coronavirus, a more digital healthcare practice.
“A more digital healthcare practice could help slow further spreads of infections, as if you have an infection and go to the doctors, you could pass it to people in the waiting area. It can also help GPs communicate more quickly and internationally, sharing advice more freely in the future.
“It can also improve the economy of the healthcare system by managing better the clinical load of frontline staff, while provide flexibility in the way citizens access healthcare services.”
Innovative digital healthcare responses come into various aspects of coronavirus, from communication, to education and patient management.
In terms of communication, clinical groups are using messaging services such as slack and WhatsApp to manage rotas as high levels of staff may be off sick or in self-isolation. They are also using social media, such as Facebook to make groups such as the ‘COVID Doctors Forum (UK)’, which on the 6th April 2020 had 14,813 members.
The group covers a range of topics, from PPE to procedures of self-isolation and lessons from colleagues internationally, as well as a number of blog posts.
There’s also been further examples in change of communication as the Discourse Digital Health Network had a page with multiple threads considering the digital response to Covid-19, as well as a webinar on the response, hosted by NHSX ,which would have previously been face to face.
Education wise many conference, training courses, post-graduate exams have been cancelled, however the need for rapid education of the healthcare workforce to deal with respiratory problems and deployment education to staff who have changed roles during the pandemic is still needed. It has therefore been carried out virtually.
Doctors in training have had their Annual Review of Clinical Progression assessments virtually, e-learning packages have also been set up much more rapidly than previously. For example, University Hospitals Coventry and Warwickshire produced a training package in just 72 hours to help staff train to deal with viral respiratory diseases.
One of the most significant changes is to patient management, in order to protect the elderly and vulnerable telemedicine consultations have taken place rather than in person.
There’s also been a rapid reaction in the MedTech industry to roll out digital tools and packages, such as EMIS, (Egton Medical Information Systems), the largest supplier of electronic health records, introducing a range of interventions, including modifying coding, alert tracking and all EMIS web GPs in the UK being able to host vide consultations for free.
Most GP practices are now offering appointments over the phone, video call or via an app.
New MRI computing technique can spot scar muscles of heart without damaging kidneys
 - Traditional MRI scans use the metal gadolinium, which resonates areas of the heart muscles that are not functioning efficiently, however gadolinium affect the Kidney function
- Traditional MRI scans use the metal gadolinium, which resonates areas of the heart muscles that are not functioning efficiently, however gadolinium affect the Kidney function
- The new 3D MRI computing technique calculates strain in heart muscles showing which muscles are not functioning enough without damaging other organs - researchers at WMG, University of Warwick have found
- The new technique is less stressful for the patient
3D MRI computing can measure strain in the heart using image registration method. Traditional method involves giving the patient a dose of gadolinium which can affect the kidney, researchers at WMG, University of Warwick have found.
MRIs are used to diagnose cardiac disease such as cardiomyopathy, heart attacks, irregular heartbeats and other heart disease.
Traditionally when a patient goes for an MRI scan they are given a dose of gadolinium, which reacts the magnetic field of the scanner to produce an image of the protons in the metal realigning with the magnetic field. The faster the protons realign, the brighter the image features and can show where the dead muscles are in the heart and what the diagnosis is.
The dose of gadolinium can have detrimental effects to other parts of the body, particularly the risk of kidney failure.
A new 3D MRI computing technique developed by scientists in WMG at the University of Warwick, published today, 28th August, in the Journal Scientific Reports titled ‘Hierarchical Template Matching for 3D Myocardial Tracking and Cardiac Strain Estimation’ focuses on Hierarchical Template Matching (HTM) technique. Which involves:
- A numerically stable technique of LV myocardial tracking
- A 3D extension of local weighted mean function to transform MRI pixels
- A 3D extension of Hierarchical Template Matching model for myocardial tracking problems
Therefore meaning there is no need for gadolinium reducing the risk of damage to other organs.
Professor Mark Williams, from WMG at the University of Warwick comments:
“Using 3D MRI computing technique we can see in more depth what is happening to the heart, more precisely to each heart muscles, and diagnose any issues such as remodelling of heart that causes heart failure. The new method avoids the risk of damaging the kidney opposite to what traditional methods do by using gadolinium.”
Jayendra Bhalodiya, who conducted the research from WMG, University of Warwick adds:
“This new MRI technique also takes away stress from the patient, as during an MRI the patient must be very still in a very enclosed environment meaning some people suffer from claustrophobia and have to stop the scan, often when they do this they have to administer another dose of the damaging gadolinium and start again. This technique doesn’t require a dosage of anything, as it tracks the heart naturally.”
Using e-health to support the challenges of an ageing population
Researchers at our Institute of Digital Healthcare have published a systematic review on e-health based active ageing interventions.
As life expectancy is at an all-time high, this type of research has become an international priority offering enormous potential to support individuals, communities, clinicians and policy makers.
Our Professor of e-Health Innovation and Head of Research, Theo Arvanitis, Dr Timothy Robbins and Dr Sarah Lim Choi Keung, worked alongside experts at University Hospitals Coventry and Warwickshire to establish the extent to which current research literature considers e-health-based and telemedicine-based active ageing interventions.
WMG research helps expand Sweatcoin capabilities
Researchers at our Institute of Digital Healthcare (IDH) have been working, with the health and fitness app Sweatcoin, to develop a new verification process that will now allow indoor steps to be tracked for the first time.
Sweatcoin monitors steps throughout the day, via an app downloaded to a smartphone. Users are rewarded with one Sweatcoin (SWC) per every 1,000 steps. The digital currency can then be redeemed for items including magazines, clothing, music downloads and even televisions.
Previously the app was only capable of tracking outdoor steps - a big disadvantage for those with active jobs indoors or even those using the gym.
The 12-month project, funded by Innovate UK, collected large amounts of data from the sensors built into smartphones in parallel with step-count data recorded using high accuracy activity monitors. Researchers on the project then used this data to create a new step-verification model to work in any environment, not just outdoors.
One of UK’s foremost NHS chief executives to lead Healthcare Systems activities at WMG
 It was announced today, Thursday 26th April 2018, that Dame Julie Moore, currently Chief Executive of University Hospitals Birmingham NHS Foundation Trust (UHB), is to become a Professor of Healthcare Systems at WMG, University of Warwick. Her new role will see her leading on a range of both research and education projects, leading collaborations with the NHS and other healthcare providers.
It was announced today, Thursday 26th April 2018, that Dame Julie Moore, currently Chief Executive of University Hospitals Birmingham NHS Foundation Trust (UHB), is to become a Professor of Healthcare Systems at WMG, University of Warwick. Her new role will see her leading on a range of both research and education projects, leading collaborations with the NHS and other healthcare providers.
Dame Julie has held the position of Honorary Professor, at WMG, since 2013. In that time she has delivered three thought provoking and informative special lectures covering topics such as ‘Is the NHS Succeeding or Failing?’
Professor Stuart Croft, Vice Chancellor of the University of Warwick said
“This is a stellar appointment. Nursing Times has described Dame Julie one of the best leaders in the NHS, and Radio 4’s Woman’s Hour has named her as one of the 100 most powerful women in the UK. I have no doubt that her new research role here with us in WMG at the University of Warwick will result in transformative research that will help enhance the delivery of healthcare across the UK.”
Healthcare technology conference hosted by the Institute of Digital Healthcare
On Thursday 3rd May 2018, the Institute of Digital Healthcare (IDH) at WMG, University of Warwick, will be hosting the Digital Health & Care and Safety of Connected Health: Improvements & Applications Conference (DICOH’18).
The national conference is being sponsored by the West Midlands Academic Health Science Network and NHS Digital.
Professor Maureen Baker CBE, Chair of the Professional Record Standards Body, Dr Cian Hughes Senior Research Scientist, DeepMind and Professor Theo  Arvanitis, Chair in e-Health Innovation and Head of Research at WMG will be joining other key experts in digital healthcare speaking at the conference.
Arvanitis, Chair in e-Health Innovation and Head of Research at WMG will be joining other key experts in digital healthcare speaking at the conference.
There will also be a tutorial on clinical IT safety organised jointly by the Institute of Digital Health and the NHS Digital.
You can get more information or register for DICOH’18 here.
WMG part of £30 million funding to help transform health through data science
 WMG, at the University of Warwick, is a key partner in the Midlands site helping to deliver a £30 million project by Health Data Research UK, to address challenging UK healthcare issues using data science, which is looking at making game-changing improvements in people’s health by harnessing data science at scale across the UK.
WMG, at the University of Warwick, is a key partner in the Midlands site helping to deliver a £30 million project by Health Data Research UK, to address challenging UK healthcare issues using data science, which is looking at making game-changing improvements in people’s health by harnessing data science at scale across the UK.
WMG will be part of the “Midlands HDR UK Substantive Site”, which will tackle the challenge of how to make NHS data more useable and accessible for research; and will develop, evaluate and apply appropriate analytical tools to NHS data in real time in order to inform decision making and improve health for both the patient and population. The Institute of Digital Healthcare (IDH), WMG will lead the Warwick part of the programme, together with colleagues from Warwick Medical School and Warwick’s Mathematics Institute.
New EUR 5 million project to transform care for multimorbid patients launched
Care for patients with multimorbid chronic conditions could be transformed by a new cloud infrastructure to be developed at the University of Warwick’s Institute of Digital Healthcare based at WMG, as part of a European project.
The system called C3-Cloud, which is led by the Institute of Digital Healthcare aims to transform current care models which are mostly fragmented, addressing chronic conditions in isolation. The researchers have been awarded EUR 5 Million to lead pilots of the system in three countries. Funded by EU Horizon 2020, 12 partners in seven countries are combining their expertise to improve care provided to patients with multimorbidity.
Patients with multimorbidity, have two or chronic conditions such as diabetes, dementia and arthritis which makes treatment more complicated and has become more prevalent among older adults as mortality rates have declined and the population has aged.
A new national database could help relieve the misery of miscarriage for thousands of women
 Researchers from the University of Warwick’s Institute of Digital Healthcare (IDH) are using data to help discover why some pregnancies fail.
Researchers from the University of Warwick’s Institute of Digital Healthcare (IDH) are using data to help discover why some pregnancies fail.
The initiative is part of the National Tommy’s Centre for Early Miscarriage Care and Research (NEMC) which is the first in the UK - and the largest in Europe. The University of Warwick has been chosen as a partner, together with the University of Birmingham and Imperial College London. The NEMC is funded by Tommy's, the baby and pregnancy charity
The team at IDH is led by Professor Theo Arvanitis, Chair in e-Health Innovation and Head of Research. He said: “Around 250,000 miscarriages occur every year, and roughly a third of women suffer more than one of these traumatic events. We'll also be creating a national database, initially by taking information from all three centres.
Microsoft’s Xbox Kinect breathes new life into respiratory assessment
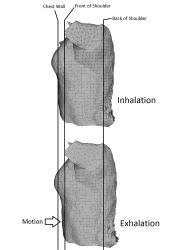 Xbox Kinects could be used in the future to assess the health of patients with conditions such as cystic fibrosis. Normally found in the hands of gamers rather than medics the Microsoft sensors could be used to assess the respiratory function of patients.
Xbox Kinects could be used in the future to assess the health of patients with conditions such as cystic fibrosis. Normally found in the hands of gamers rather than medics the Microsoft sensors could be used to assess the respiratory function of patients.
Researchers at the Institute of Digital Healthcare, WMG, University of Warwick and the Institute of Inflammation and Ageing, University of Birmingham and Heart of England NHS Foundation Trust (HEFT) have developed a method of using the devices. The system consists of four Kinect sensors which are capable of quickly creating a 3D image of a patient’s torso. This enables physicians to measure and assess how a chest wall moves. In tests it has proven to be as accurate as a patient breathing into a spirometer - the current method used - but providing additional information about the movement of the chest, which could help in identifying numerous respiratory problems.
The project lead, Dr Chris Golby at the Institute of Digital Healthcare, said: “We have developed a low-cost prototype which provides a more comprehensive measurement of a patient’s breathing than existing methods.”
Their work is detailed in their paper Chest Wall motion Analysis in Healthy Volunteers and Adults with Cystic Fibrosis using a Novel Kinect-based which is published in Medical & Biological Engineering & Computing.

